by Anthony Hennen
The owner of a Pennsylvania drug and alcohol treatment facility has pleaded guilty to a Medicaid fraud case that netted his organization $12 million over three years in an illegal kickback scheme.
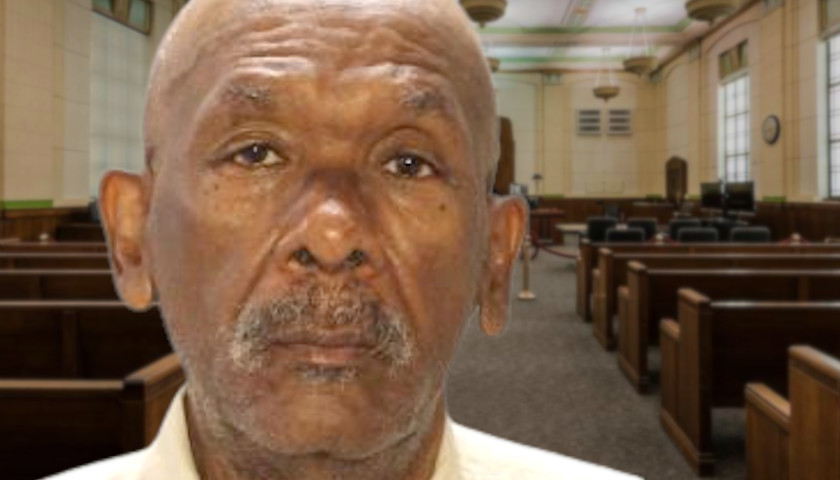
The attorney general’s office announced the plea of Dr. Lloyd Reid, the owner of Southwest Nu-Stop Philadelphia Inc., which came about from a joint investigation of the office’s Medicaid Fraud Control Section and the U.S. Department of Health and Human Services.
Philadelphia’s Community Behavioral Health office had cited Southwest for low standards of care in the past, and a patient fatally overdosed in January 2020 in a Southwest treatment facility.
“People with substance use disorder who stayed in these recovery homes were forced to attend certain substandard, outpatient treatment programs,” a press release noted. “Those outpatient treatment programs paid kickbacks to the recovery homes in return for those homes funneling patients to them, rather than giving the patients choice.”
From December 2016 to June 2019, more than $12,662,864 in Medicaid funds were sent to Southwest to provide drug and alcohol treatment. Reid then paid recovery homes over $1,178,453 in kickbacks.
The more people ushered into programs, the more Southwest could receive from Medicaid funds.
“Patients were required to live in overcrowded recovery homes and attend overcrowded group therapy sessions, including up to double the number of suggested patients for a group therapy session,” the attorney general’s office noted. “Stripping the patients of their freedom of choice, the recovery homes threatened the residents with life on the streets if they choose to attend treatment at a different facility.”
Even before the fatal overdose, Philadelphia’s CBH unsuccessfully tried to remove Southwest from its provider network.
Since 2017, when Josh Shapiro became attorney general, the Medicaid Fraud Control Section has made 560 arrests and more than $16 million in court-ordered restitution.
Medicaid fraud is a significant financial burden on the state and federal level. The U.S. Government Accountability Office estimated that more than $57 billion of improper payments were made through Medicaid programs in 2019. The federal government funds 75% of Pennsylvania’s Medicaid Fraud unit, about $9 million for fiscal year 2022.
Anthony Hennen is a reporter for The Center Square. Previously, he worked for Philadelphia Weekly and the James G. Martin Center for Academic Renewal. He is managing editor of Expatalachians, a journalism project focused on the Appalachian region.