by James D. Agresti
Overview
In a terse essay titled “Science and Dictatorship,” Albert Einstein warned that “Science can flourish only in an atmosphere of free speech.” And on his deathbed, Einstein cautioned, “Whoever is careless with the truth in small matters cannot be trusted in important affairs.”
With reckless disregard for both of those principles, powerful government officials and big tech executives have corrupted or suppressed the central scientific facts about face masks. The impacts of this extend far beyond the issue of masks and have caused widespread harm and countless deaths.
Despite the fog of contradictory claims and changing government guidelines, dozens of scientific journals have published consistent data that establish these facts:
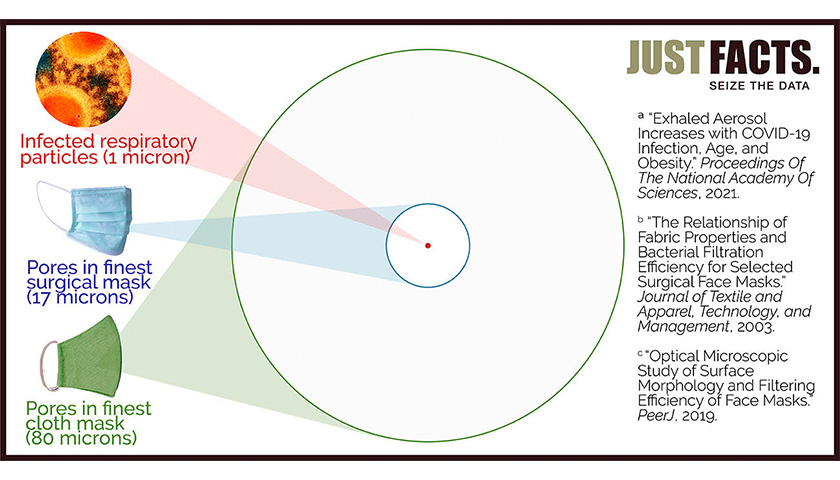
- Covid-19 is mainly spread by microscopic aerosols generated by breathing, talking, sneezing, and coughing. The vast bulk of these infectious aerosols easily penetrate common masks because 90% of the aerosols are less than 1/17th the size of pores in the finest surgical masks, and less than 1/80th the size of pores in the finest cloth masks.
- Aerosols are light enough to stay airborne for minutes or hours, and hence, they also travel freely through gaps around the edges of cloth and surgical masks.
- Governments enacted mask mandates based on the false assumption that C-19 is mainly transmitted by large droplets generated by coughing, sneezing, and spittle. These droplets are bigger than the pore sizes of most masks and only remain airborne for a few seconds after they are emitted.
- For more than a year, the World Health Organization and the U.S. Centers for Disease Control and Prevention denied and downplayed the threat of aerosol transmission while issuing guidelines that don’t amply prevent it. This enabled C-19 to decimate the most vulnerable members of society, like those in hospitals and nursing homes.
- The CDC and WHO quietly admitted in the spring of 2021 that aerosols pose a major threat of transmission but have still not adequately updated their guidelines to reflect this reality. This has allowed countless preventable deaths to continue.
- The risk of aerosol transmission can be greatly reduced by disinfecting air with ultraviolent (UV) light, which is part of the energy spectrum emitted by the sun. This simple and safe technology neutralizes airborne microbes and has been successfully used to control the spread of contagious respiratory diseases for more than 80 years.
- Randomized controlled trials—which are the “gold standard” for clinical research—have repeatedly measured the effects of masks on preventing the spread of contagious respiratory diseases. These trials have found inconsistent benefits from N95 masks in healthcare settings and no statistically significant benefits from any type of mask in community settings.
- The only randomized controlled trial that evaluated cloth masks found that mandating them causes significant disease transmission in high-risk healthcare settings.
- Observational studies—which are a weaker form of evidence than randomized controlled trials—find that masking schoolchildren provides negligible or no benefits.
- Lab studies—which are the weakest form of clinical evidence—don’t support the notion that surgical or cloth masks reduce the transmission of Covid-19.
- Masks of all types have negative impacts on some people, including headaches, difficulty breathing, increased cardio-pulmonary stress during exercise, marked discomfort, and weakened social bonds.
- Because humans create carbon dioxide as they breathe, the CO2 concentration of the air they exhale is about 100 times higher than in fresh air. Masks restrict airflow and thus cause the wearers to rebreathe some of the air they exhale.
- The average CO2 concentrations inhaled by people wearing N95 masks range from 2.6 to 7.0 times OSHA’s work shift limit for CO2. These levels cause headaches and chest pains in some people.
- The average CO2 concentrations inhaled by people wearing cloth and surgical masks range from 2 to 3 times the government CO2 limits for classrooms in many countries. These levels may impair certain high-level brain functions like initiative, strategic thinking, and complex decision-making.
The leaders of big tech corporations like Facebook, Twitter, and Google/YouTube have empowered government officials who misled the public about every matter above and others. Together, they continue to do so by engaging in actions that resemble common disinformation tactics. These include but are not limited to cherry-picking, censorship, muddying the waters, citation bluffs, non-sequiturs, half-truths, and outright falsehoods.
Opinions Are Not Science
A very common and naive talking point about masks is that “experts say” they reduce the spread of Covid-19. Such statements are oblivious to the reality that other experts disagree with that opinion, like these for example:
- Dr. Erica Shenoy, the Associate Chief of the Infection Control Unit at Massachusetts General Hospital, along with four other medical professionals, wrote in the New England Journal of Medicine that “wearing a mask outside health care facilities offers little, if any, protection from infection.”
- Dr. Martin Kulldorff, a Professor of Medicine at Harvard Medical School, has stated, “Children should not wear face masks” because “they don’t need it for their own protection and they don’t need it for protecting other people either.”
- Tamara van Ark, a public minister in The Netherlands, announced the conclusion of the nation’s National Institute for Health as follows: “Because from a medical perspective there is no proven effectiveness of masks, the Cabinet has decided that there will be no national obligation for wearing non-medical masks.”
- Dr. Joseph Allen, an associate professor and the director of the Healthy Buildings program at Harvard University, wrote, “The truth is, for kids, Covid-19 is like the flu, and we don’t make kids wear masks in school for that.”
- Dr. Shamez Ladhani, a professor of pediatric infectious diseases and vaccinology at St. George’s University of London, wrote that masking may help reduce Covid-19 transmission when used with other “infection control measures, but I have yet to see any convincing evidence that masking in and of itself significantly contributes to reducing infection and transmission” in schools and other institutional settings.
- Dr. Jay Bhattacharya, a Professor of Medicine at Stanford University, said, “On net, I think the masks not only have not been effective, but have been harmful.”
- Dr. Lisa Brosseau and Dr. Margaret Sietsema, researchers specializing in infectious diseases and respiratory protection, wrote, “There is no scientific evidence” that “cloth or surgical masks” are “are effective in reducing the risk of SARS-CoV-2 transmission.”
Regardless of what any experts say or how many say it, their opinions do not constitute scientific facts. Yet, journalists, commentators, and “fact checkers“ often treat the mere opinions of selected experts as “facts” or “science,” and politicians use the phrase “science says“ as if it magically turns claims into facts.
Such misuse of the word “science” has been a longstanding problem. As the renowned physicist Richard Feynman remarked half a century ago, “When someone says, ‘Science teaches such and such,’ he is using the word incorrectly.” People who are actually discussing science, explained Feynman, don’t “say science has shown”—but rather “this experiment, this effect, has shown.”
This article presents actual science, and there is no substitute for it when lives are on the line. Although greatly condensed from more than 500 hours of research, these thoroughly vetted facts will take more than an hour for most people to read. This is the price of being informed instead of indoctrinated.
Easy vs. Hard Measurements
Because masks have been used in operating rooms for more than a century, many studies have been conducted on them dating back to at least 1935. One might assume that these studies quickly found benefits given that the main purpose of surgical masks is simple: to prevent bacteria from the mouths and noses of surgeons from falling into the open wounds of their patients.
Yet more than half a century later, a 2001 paper in the Journal of Hospital Infection reviewed all known studies about “surgical face masks in the operating theatre” and found that their “effectiveness remains unresolved.” A 2016 paper found the same. Such outcomes commonly occur when the effects of something are very minimal or difficult to measure.
Measuring the impact of masks on the spread of infectious diseases in homes and public places is considerably harder than in operating rooms. This is because such settings are far more diverse and less controlled than operating rooms, which are subject to strict infection control protocols.
These facts suggest that cocksure and simple-minded statements like “masks work” should be treated with skepticism.
Strong vs. Weak Studies
In 2019—the year before C-19 pandemic began—the World Health Organization published a lengthy analysis of different strategies to limit the impact of the flu in “community” or “non-healthcare“ settings. The analysis found “there was no evidence that face masks are effective in reducing transmission” of the flu in these situations.
Covid-19 differs from the flu, and one of the main differences is that C-19 is much more transmissible. This raises the question: How can masking reduce the community spread of C-19 when there is “no evidence” that it does so for the flu?
Fortunately, a vital tool to answer that question is provided in WHO’s supplement to the same analysis. In it, WHO correctly notes that the key to sorting out masses of studies is to rank the “quality of evidence” from strongest-to-weakest in the following order:
- Randomized controlled trials (RCTs): These are studies in which people are randomly assigned to receive or not receive a certain treatment. Done properly, these are the “gold standard“ for clinical research because they provide “a rigorous tool to examine cause–effect,” which “is not possible with any other study design.” That is why the medical textbook Rutherford’s Vascular Surgery calls RCTs “the pinnacle in clinical design.”
- Observational studies: These studies observe the outcomes of people who have not been randomly assigned a certain treatment. Unless their results are mathematically and logically overwhelming, observational studies can “rarely” determine the effects of a treatment because a host of other factors are always at play when it comes to people’s health. For example, measuring the C-19 death rates of nations with and without mask mandates cannot determine the effects of the mandates because many factors impact C-19 death rates. As documented in a 2018 paper in the European Heart Journal, “it is not possible to make reliable therapeutic inferences from” observational studies.
- Laboratory and simulation studies. These are experiments conducted under artificial conditions and are typically the weakest form of clinical evidence. As explained by the UK’s Department of Health, such “studies provide only theoretical evidence” because they “are run in controlled environments that may not accurately reflect the behaviours that we observe in real life.” Likewise, a 2020 paper in a German medical journal explains that such studies can “provide important mechanistic insights” about Covid-19 transmission, but they “never approximate real-world conditions,” and thus, they should “not directly inform policy decisions.”
The quality gaps between those types of studies are so great that WHO adopted a “general principle” to “not review simulation studies” if observational studies were available and to “not review observational studies or simulation studies” if RCTs were available.
However, WHO broke that rule for masks while explaining that even though all “ten RCTs” showed “no evidence that face masks are effective in reducing transmission” of the flu, “there is mechanistic plausibility for the potential effectiveness of this measure.” Thus, WHO flouted its own principle and “conditionally recommended” that asymptomatic people wear face masks “in severe epidemics or pandemics, to reduce transmission in the community.”
Relevance
Beyond the general quality of a study, another important factor to consider is how applicable it is to the issue at hand. Studies on trained nurses who wear N95 masks to reduce the spread of tuberculosis during 10-minute interactions in sanitized hospital wards are less relevant to the present issue than studies on 5-year-olds wearing cloth masks for six hours in poorly ventilated schoolrooms during the C-19 pandemic.
Of great import for understanding the coming facts, the three main types of masks from the highest-to-lowest quality are:
- N95 masks or respirators, which are mainly intended to prevent wearers from inhaling fine aerosols and microscopic particles. These are supposed to be used only once, must meet strict filtration standards, and must be moldable to each user’s face to form a tight seal. Because N95s heavily restrict breathing and “may place a burden on an employee’s health,” OSHA requires employers to conduct a medical evaluation of each employee who wears them.
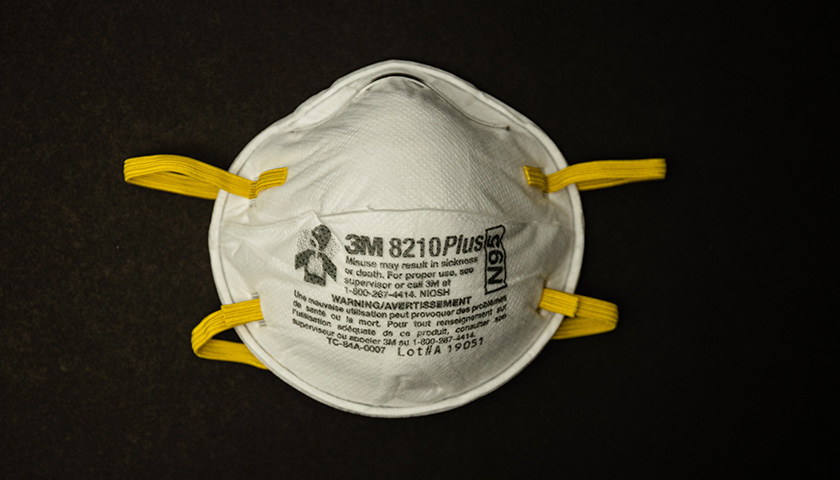
- surgical or medical masks, which are primarily designed to prevent wearers from spraying liquid droplets and large particles on other people. The FDA’s Covid-19 guidance for these masks states that they cannot be labeled “for antimicrobial or antiviral protection” and cannot make “filtration claims” for particles of any size. Per a 2013 paper in the Journal of Occupational and Environmental Hygiene, surgical masks have “poor filtration” and a “poor fit,” and thus, they “cannot be expected to significantly reduce the inhalation of infectious aerosols.” They are supposed to be used only once.
- cloth masks, which are made of common fabrics that tend to be highly permeable. These masks were already worn before the C-19 pandemic in developing countries because they are inexpensive and can be used more than once. The CDC says they should be washed at least once a day, and washing them makes the fabrics even more permeable.

In July 2020, the Journal of the American Medical Association published a commentary titled “Universal Masking to Prevent SARS-CoV-2 Transmission—The Time Is Now.” The authors—all of whom were CDC employees—argued that the benefits of using masks during surgery are relevant to the general public. This leap of logic conflates surgical masks with cloth masks, sterilized operating rooms with subways, and open wounds with people’s faces.
The authors also claimed—without citing any research—that it would be “absurd” to conduct surgery without masks “because it is known that use of face coverings under these circumstances reduces the risk of surgical site infection caused by microbes generated during the surgical team’s conversations or breathing.”
That assertion is at direct odds with the strongest, most relevant research on this issue. This was summarized in a 2016 paper published by “the leading journal and database for systematic reviews in health care.” After conducting an extensive search for all available RCTs on the use of surgical masks to prevent wound infections, the authors located three trials and found “there was no statistically significant difference in infection rates between the masked and unmasked group in any of the trials.”
This straightforward example dramatically illustrates how the claims of “experts” published in one of the world’s leading medical journals can be at odds with documented facts. Yet with callous disregard for the facts—and thus the wellbeing of people—Google/YouTube, Facebook, and Twitter have banned factual statements about masks that conflict with the opinion of their chosen experts.
Gold Standard Studies
Like the 2019 analysis of RCTs by the World Health Organization, other comprehensive analyses of gold standard studies have found no evidence that low-quality masks reduce the spread of the flu in community settings. Moreover, such studies have found limited evidence that any type of mask protects against the flu in any setting:
- In 2010, the journal Epidemiology & Infection published a “systematic review” of studies that examined the use of “face masks to prevent transmission of influenza virus,” including several RCTs. The analysis found that “while there is some experimental evidence that masks should be able to reduce infectiousness under controlled [i.e., lab] conditions, there is less evidence on whether this translates to effectiveness in natural settings” and “little evidence to support the effectiveness of face masks to reduce the risk of infection.”
- In 2011, the journal Influenza and Other Respiratory Viruses published a “systematic review of the scientific evidence” on the “use of masks and respirators to prevent transmission of influenza.” The authors examined eight RCTs and found:
- that “none of the studies we reviewed established a conclusive relationship between mask/respirator use and protection against influenza infection.”
- “there is a limited evidence base to support the use of masks and/or respirators in healthcare or community settings.”
- “some useful clues” that “correct and consistent wearing of masks/respirators may improve their effectiveness,” but “this remains a major challenge” in “the context of a formal study and in everyday practice.”
- In May 2020, a CDC journal named Emerging Infectious Diseases published a “systematic review” of 10 RCTs that “reported estimates of the effectiveness of face masks in reducing” the spread of the flu in community settings. A “pooled analysis” of their results found “no significant reduction in influenza transmission with the use of face masks,” regardless of whether they are “worn by the infected person” to protect others, or if they are worn by “uninfected persons” to protect themselves from people who are infected.
All of those flu RCTs are highly relevant to Covid-19 because:
- both diseases are transmitted by RNA viruses that produce respiratory tract infections.
- more than 87% of virus-laden respiratory particles exhaled by people with either disease are less than 1 micron in diameter. These can easily penetrate surgical and cloth masks because the average pore sizes of:
 Broadening the research beyond the flu to other types of infectious respiratory diseases, RCTs have found inconsistent evidence that higher-quality masks may help in healthcare settings but no statistically significant evidence that any type of mask helps in community settings:
Broadening the research beyond the flu to other types of infectious respiratory diseases, RCTs have found inconsistent evidence that higher-quality masks may help in healthcare settings but no statistically significant evidence that any type of mask helps in community settings:
- In 2017, the journal Clinical Infectious Diseases published “a systematic review and meta-analysis” about the “effectiveness of masks and respirators against respiratory infections in healthcare workers.” It found that RCTs “indicated a protective effect” from masks but that the “evidence is sparse and findings are inconsistent within and across studies.” It also found that “N95 respirators conferred superior protection” to lower-quality masks.
- In March 2020, the Journal of Evidence-Based Medicine published a systematic review of six RCTs on masks published in the past five years. It found “there were no statistically significant differences in preventing laboratory-confirmed influenza, laboratory-confirmed respiratory viral infections, laboratory-confirmed respiratory infection and influenza-like illness using N95 respirators and surgical masks.” It only compared these masks to one another and not to using no masks.
- In June 2020, the Annals of Internal Medicine published a “living rapid review” of mask studies involving viral respiratory infections. The review found:
- 8 RCTs in household settings that showed “surgical masks were not associated with decreased risk” for respiratory disease regardless of whether masks were worn by sick people, other people in their households, or everyone.
- 2 RCTs in college dorms that showed “no significant differences between a surgical mask versus no mask and risk for influenza-like illness.”
- 2 RCTs among pilgrims to Mecca that showed surgical masks “were not associated with decreased risk for infections,” even when healthy and sick people lived in the same tents.
- In April 2021, the authors of the above living review updated their research a fifth time to incorporate all newly published mask studies. Only one of these was an RCT, and it found that wearing a surgical mask in community settings was associated with a “small” and statistically insignificant reduction in the odds of catching C-19. More precisely, the study found with 95% confidence that people assigned to wear surgical masks in Denmark had “a 46% reduction to a 23% increase” in C-19 infections compared to those who were assigned to not wear a mask. Of special import to the next analysis below, each mask wearer was given “a supply of 50 surgical masks” and “instructed to change the mask if outside the home for more than 8 hours.”
- In July 2020, the Center for Evidence-Based Medicine at Oxford University published an analysis of 12 RCTs on masks. It found that:
- “masks alone have no significant effect in interrupting the spread” of the flu or flu-like illnesses “in the general population, nor in healthcare workers.”
- one of the largest RCTs—which studied 1,607 healthcare workers in 74 “high-risk wards” of 14 Vietnamese hospitals—showed that people assigned to wear cloth masks were about 13 times more likely to contract a respiratory infection than those who wore surgical masks.
The last of those studies is particularly relevant to C-19 mask mandates because:
- it is the only RCT that evaluated cloth masks, the most-commonly worn mask during the C-19 pandemic.
- 85% of all laboratory-confirmed infections in the study were rhinoviruses, which share a key trait with C-19: both can be transmitted by fine particles (called aerosols) that easily penetrate cloth masks.
- the workers who were assigned to wear cloth masks got infected at 3.49 times the rate of workers who were told to “continue with their normal practices, which may or may not have included” wearing cloth or surgical masks. Though “almost all” of these workers wore some type of mask at certain times, only 24% of them wore a mask for more than 70% of their working hours. In other words, the people mandated to wear cloth masks were 3.5 times as likely to become infected than those who wore masks occasionally.
When the RCT on cloth masks was published in 2015, the lead author of the study, Raina MacIntyre of the University of New South Wales (Australia)—stressed “it is important for global disease control that the use of cloth masks be discouraged in high-risk situations.” However, she and some of her coauthors began backpedaling five years later in 2020 when governments began mandating masks for C-19. MacIntyre and company did this by:
- claiming without evidence that “the physical barrier provided by a cloth mask may afford some protection”—despite the results of their own paper which:
- found via laboratory testing that particle “filtration was extremely poor (almost 0%) for the cloth masks.”
- “caution against the use of cloth masks.”
- claiming in a 2020 paper in the International Journal of Nursing Studies that eight RCTs showed community masking “appeared to be effective,” even though:
- a May 2020 paper in the CDC journal Emerging Infectious Diseases examined the very same RCTs (plus two others) and found “no significant reduction in influenza transmission with the use of face masks” in a “pooled analysis.”
- not one of the eight RCTs they cited found a statistically significant positive impact from masking.
The last of those papers—which was coauthored by MacIntyre and published by the CDC—buries the results of the RCT two-thirds of the way into a lengthy paragraph. There, the authors reveal that the “intent-to-treat analysis”—which is the actual RCT—“showed no significant difference” in outcomes between the people who were assigned to wear masks and not wear masks.
While concealing the gold standard results of their own study, MacIntyre’s team focused their analysis on a subset of people who had the highest “adherence to mask use.” This violates the very essence of RCTs, which are supposed to be “randomized control trials.” Randomization is the linchpin that allows these studies to determine cause and effect.
For that reason and others, Dr. Alyson Haslam of the Oklahoma State University Center for Health Sciences Research publicly criticized MacIntyre and her colleague (Dr. Abrar Ahmad Chughtai) for spreading “incorrect/biased summaries of published articles.”
MacIntyre and Chughtai replied without confronting the central fact of this matter: people who were more diligent about wearing masks may have taken other precautions to avoid getting sick, like social distancing or washing their hands more often. In other words, their conclusion that masks “appeared to be effective” is not based on RCTs, even though their paper claims to be an analysis of “randomised controlled trials.”
Furthering that misleading impression, MacIntyre and Chughtai end their reply to Haslam by declaring that “a WHO-commissioned study has shown that masks reduce the risk of infection with beta-coronaviruses by 85%, and are equally protective in community and healthcare settings.” However, that WHO-commissioned study is not an RCT but an analysis of observational studies. Thus, it cannot prove that “masks reduce the risk” of anything. That is precisely why the authors of the study write that their results have “low certainty.”
Compounding the deceit, the CDC published a study in July 2020 that cites MacIntyre and Chughtai’s paper while claiming that they analyzed “randomized trials and concluded that use of face masks and respirators appeared to be protective in both health care and community settings.” Again, none of those findings are actually based on RCTs.
Beyond the CDC’s false portrayal of non-RCTs as RCTs, the same CDC study ignores the actual RCTs, all of which show no statically significant benefit from community masking. To reiterate, these studies are systematically analyzed in papers and reports published by:
- Emerging Infectious Diseases (the CDC’s own journal).
- the journal Epidemiology & Infection.
- the Center for Evidence-Based Medicine at Oxford University.
- the journal Influenza and Other Respiratory Viruses.
- the journal Clinical Infectious Diseases.
- the World Health Organization.
- the journal Annals of Internal Medicine.
The misinformation spread by MacIntyre, Chughtai, and the CDC cannot fool informed people with time to vet it, but it can muddle the issue enough to prevent all but the most tenacious researchers from finding the facts. Combined with the power of big tech corporations who suppress facts that contradict the CDC’s claims about masks, this is more than enough misinformation and censorship to keep the vast bulk of people in the dark.
In summary, a large array of gold-standard studies have found inconsistent benefits from higher-quality masks in healthcare settings and no statistically significant benefits from any type of mask in community settings. Crucially, the only RCT to evaluate cloth masks found that mandating them causes significant disease transmission in high-risk healthcare settings.
Disregarding RCTs
Faced with a mountain of RCTs that undercut their claims, proponents of community masking ignore or deceitfully dismiss them. For example, the CDC’s “Science Brief” on “Community Use of Cloth Masks” does not rely on a single RCT to support its claim that “universal masking” reduces the spread of C-19.
Instead, the CDC ignores all but two of the RCTs, which it brushes aside in a single paragraph. One of these is the lone RCT on cloth masks, and the manner in which the CDC tries to spin it is a textbook case of junk science:
- The CDC declares that the study was “unblinded,” which could bias “self-reporting of illness.” Blinding is a research technique in which people involved with a study don’t know who is receiving a treatment (and who is not) so that they don’t react differently. The duplicity of the CDC’s criticism is exposed by the simple fact that all non-lab studies of masks are unblinded because the participants can easily tell if they are wearing a mask and what type of mask they are wearing. As the study states, “The laboratory results were blinded and laboratory testing was conducted in a blinded fashion,” but because “facemask use is a visible intervention, clinical end points could not be blinded.” Yet, the CDC misleads by singling out this one study as “unblinded,” even though this is the case with every real-life study of masks.
- The CDC alleges that the study is flawed because the participants created “the risk of infection” by handwashing and reusing their masks. That rationalization ignores the fact that people who use cloth masks in community settings also handwash and reuse their masks. Furthermore, each of the study participants were “provided with five masks,” told to wash them “with soap and water every day,” and “supplied with written instructions” on how to do this. If healthcare professionals in a clinical study became infected as a result of this protocol, why wouldn’t the general public?
- The CDC claims that the study suffers from “limited source control as hospitalized patients and staff were not masked.” Source control is using masks to prevent viruses from exiting (as opposed to entering) people’s mouths and noses. Contrary to the CDC’s complaint, the study was designed to address this issue by using a method called “cluster randomization.” This involves giving “the same treatment” (i.e., mask) to people who work together. The authors of the study explain that they used this method to find out if the “prevention of one infection in an individual can prevent a chain of subsequent transmission” to their coworkers. In addition, the study included a tightly controlled lab experiment on cloth masks which found that their “filtration was extremely poor” and 97% of all respiratory particles passed right through them. (More details about this are provided below in the section on laboratory studies.)
- The CDC argues that the study lacked “a true control (no mask) group for comparison.” That is a blatant half-truth because the CDC neglects to mention that people who were assigned to wear cloth masks were 3.49 times as likely to become infected than people who were assigned to “continue with their normal practices” of wearing masks occasionally. For the record, the study didn’t have a completely maskless group because a medical board “deemed it unethical to ask participants to not wear a mask.” Ironically, the results of the study suggest it is unethical to ask people to wear a cloth mask, which the study required of them.
- Finally, the CDC states, “A follow up study in 2020 found that healthcare workers whose cloth masks were laundered by the hospital were protected equally as well as those that wore medical masks.” As evidenced by the coming facts, that statement epitomizes the adage, “If you torture the data enough, it will confess to anything.” Here again, MacIntyre and Chughtai are complicit:
-
- In June 2020, MacIntyre and Chughtai submitted a follow-up paper to their 2015 RCT on cloth masks (the same one that found mandating cloth masks amplifies disease transmission in high-risk healthcare settings).
- Their new 2020 paper was based on the same study as the original 2015 paper, which examined three measures of infection. Without explanation, however, the new paper failed to examine the only “statistically significant” measure of infection found by the original paper. Instead, the new paper only examined one of the measures that were “not statistically significant.” Just Facts asked MacIntyre why they made this baffling choice and has not received a reply.
- Only 22 people in the original study used “hospital laundry” as their sole method of washing, and the new paper does not report the infection rate for this group. Instead, it lumps them in with 91 people who used a combination of laundry and handwashing. Then it uses a statistical “technique” to supposedly determine whether infections among these people are counted in the laundry group or handwashing group.
- The new analysis suffers from a fatal flaw that a 2016 paper in the journal Nature calls one of the “most common” “invalidating errors” that plague peer-reviewed research: failing to incorporate the “number of clusters” (not just the number of individuals) into analyses of cluster randomization trials.
- Most simply and perhaps most importantly, the subjects in the study were not randomly assigned to wash their masks by hand or by hospital laundry. This means the new analysis is not an RCT. Yet, the authors included the words “analysis of a randomised controlled trial” in the title of their paper, giving the polar opposite impression.
Bottom line: the manner in which certain people disregard and twist gold-standard studies on masks says little about the studies but reveals a great deal about the people.
Observational Studies
To repeat, observational studies cannot determine the effects of medical treatments except in rare cases. This is because many factors influence people’s health, and without an RCT, it is impossible to isolate the effects of any one factor from all of the others. A simple but vivid example that highlights this reality is the number of C-19 deaths in Texas before, during, and after its mask mandate:
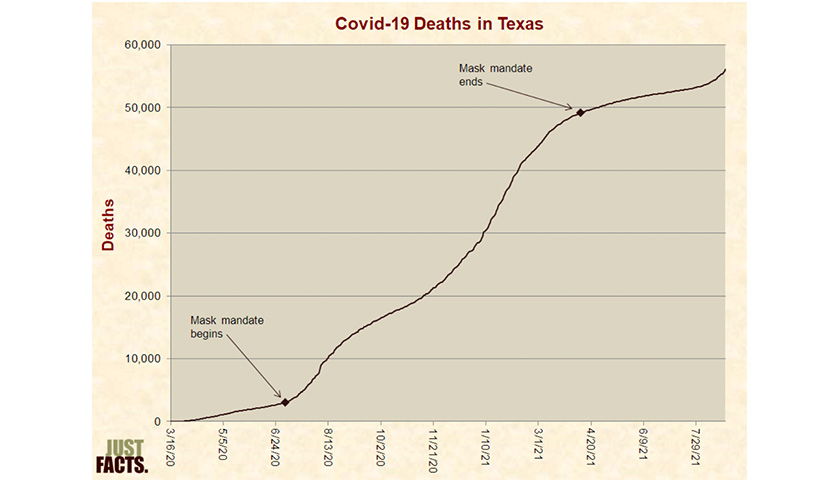
This observational data shows that the rate of C-19 deaths was consistently higher during the mask mandate, but deaths began rising again more than three months after the mandate ended. In isolation, these trends look like the mask mandate did nothing to stem the tide of C-19 deaths and may have even intensified them, but the reality is that countless other factors are involved, like:
- vaccine uptake,
- waning vaccine efficacy over time,
- the number of people with naturally acquired immunity,
- social distancing mandates and behaviors,
- the use of therapeutic treatments,
- superspreader events,
- nursing home and hospital protocols,
- holiday gatherings,
- vacations,
- virus variants,
- weather changes that lead people to spend more time indoors or outdoors,
- the number of living people who remain vulnerable to C-19,
- and the lag times associated with all of the foregoing dynamics.
Without accounting for those and many other variables, there is no way to objectively measure the effects of masks on C-19 deaths. RCTs naturally do this, but an observational study cannot.
Researchers often use statistical techniques to “control” for such variables in observational studies, but these methods cannot rule out the possibility that other factors are at play. Also, the techniques used to perform such analyses are prone to pitfalls.
All of these realities boil down to one of the most important and neglected facts of science: association does not prove causation. This is commonly taught in high school math, but it is routinely ignored by commentators, journalists, and Ph.D.’s.
Because observational studies can only determine associations, they cannot be used to draw firm conclusions about causation unless the results are mathematically and logically overwhelming.
After investing more than 500 hours of research on masks, Just Facts found only one observational study that addresses their necessity and rises to that level of certainty. Published by the New England Journal of Medicine in February 2021, the study was conducted in Sweden from March to June of 2020 when the nation experienced substantial growth in C-19 deaths:
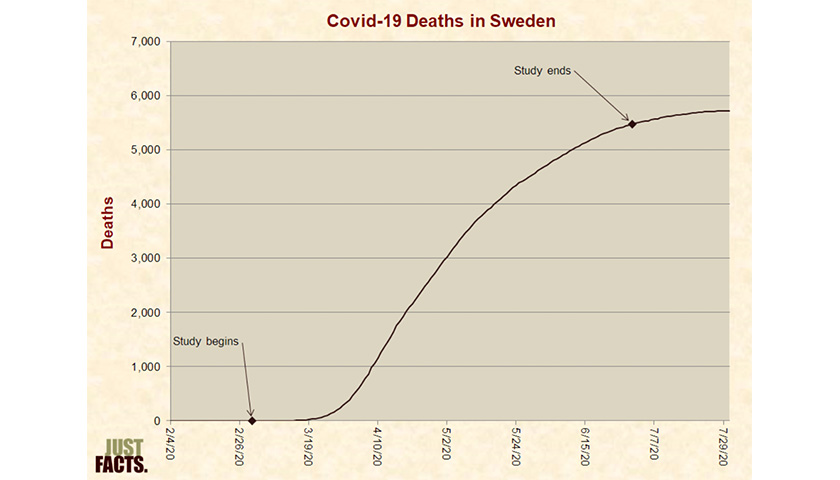
Unlike smaller studies with convenience samples that may not reflect the broader population, this study included all of Sweden’s 1.95 million children aged 1 to 16 years who attended school in the spring of 2020. During this period:
- masks were not required or even “encouraged,” and thus, they were “rarely used.”
- C-19 vaccines were not available.
- there were “no imposed class-size reductions.”
- there was “no quarantine“ of people exposed to C-19 unless they showed “symptoms of infection.”
The study found that:
- “no child with Covid-19 died.”
- 1 out of every 130,000 children were admitted to an ICU while infected with C-19, including those admitted for reasons that had nothing to do with C-19 like cancer and accidents.
- 1 out of every 5,000 teachers were admitted to an ICU while infected with C-19, a rate half that of other professions.
Strengthening those results, the Public Health Agency of Sweden published a study in July 2020 that found “no difference” in the incidence of C-19 infections among school-aged children in Finland and Sweden—even though Finland closed its schools, while Sweden left them open without mandating or encouraging masks.
Likewise, a March 2021 paper in the Proceedings of the National Academy of Sciences:
- published the results of an observational study of C-19 outcomes among parents and teachers of Swedish schoolchildren aged 14–16 (whose schools remained open) versus students aged 17–19 (whose schools closed).
- begins by reporting that “open schools resulted in a small increase in infections among parents” and a doubling of infection rates among teachers, which “spilled over to their partners.”
- reveals six pages into the paper that those results may be due to “differences between households”—but assuming they are not—there would have been “6.5 fewer deaths, 5 among parents and 1.5 among teachers and their partners” in the entire nation of Sweden if it had closed every school for students aged 14 to 16.
In combination, those massive observational studies provide fairly strong but not definitive evidence that closing schools or masking schoolchildren provide negligible or no benefits. In combination with the throng of RCTs on masks, this conclusion becomes nearly undeniable.
While ignoring this wealth of strong, comprehensive studies, the CDC’s Covid-19 guidance for K-12 schools declares:
- “Masks should be worn indoors by all individuals (age 2 and older) who are not fully vaccinated.”
- Even if vaccinated, all “passengers and drivers must wear a mask on school buses” with few exceptions.
- “Based on the needs of the community, school administrators may opt to make mask use universally required (i.e., required regardless of vaccination status) in the school.”
The CDC claims that those policies are “based on current scientific evidence” while linking to a CDC “Science Brief” which cites observational studies that prove nothing of the sort. For example, the brief cites:
- a contact-tracing study of 90,000 students and staff in a sample of North Carolina schools:
- that operated with less than half of their students present each day and had mask and social distancing requirements.
- where the researchers could not “determine the relative effectiveness of any specific school policies.”
- in which C-19 “testing could not be universally enforced” because students were “not required to return to school” at any time.
- where the researchers “were not able to analyze incidence of child-to-child or adult-to-child transmission” due to “confidentiality concerns.”
- a study which concludes that reopening schools was probably not “a driver of the second Covid-19 wave in Italy” and:
- found that the C-19 infection rate “among students was lower than in the general population.”
- reports that both students and adults were subject to a “mandate for universal mask wearing outside home.”
- found that “school age children and adolescents” are “largely spared from the clinical consequences” of C-19, “are less likely to transmit it,” and often “harbor antibodies” that may protect them from it.
- states that “decision makers, popular press and public opinion in Italy” wrongly “ascribed the second wave of COVID-19 to school reopening” and made “deprecating comments” about teens “who would not follow the strict rules at school or outside them.”
After proclaiming that those and other studies demonstrate the “success” of mask mandates, the CDC cites two observational studies that supposedly show “inconsistent mask use may have contributed to school-based outbreaks.” Absurdly, these consist of:
- a study of a C-19 outbreak in a single Israeli school during a heat wave when:
- the nation’s “Ministry of Health exempted schoolchildren from facemasks” for three days.
- the students and teachers were confined to “crowded” classrooms containing 35 to 38 students.
- windows and doors were closed while “air-conditioning functioned continuously in all classes.”
- “distancing among students and between students and teachers was not possible.”
- a study of C-19 infections “in a single school district” in Georgia where:
- “nine clusters” of Covid-19 cases occurred among “13 educators and 32 students at six elementary schools.”
- “the school district mandated in-classroom mask use except while eating, and both reported and observed compliance during site visits was high.”
- “interviews with parents, educators, and principals” indicated a “lack of or inadequate mask use by students” in five of the nine clusters.
In other words, the CDC blames a handful of C-19 cases on less-than-perfect mask usage in a school district where masks were required, compliance was “high,” and interviews failed to detect even slight non-compliance in four of the nine clusters that caught C-19. Yet, the CDC ignores two million students in Sweden who rarely wore masks, rarely became infected, and not one of whom died from C-19.
After closing out the section on masks, the same CDC “Science Brief” craftily slips the following statement into a section on “Physical Distancing”:
K–5 schools in Norway had minimal child-to-child and child-to-adult transmission with masks only required for adults, one meter between all individuals, and two meters between student cohorts.
In reality, the study mentions masks only once and states: “Use of face masks is not recommended in schools in Norway.” This means that C-19 transmission was minimal in schools that practiced social distancing but did not require or even recommend masks. Put bluntly, the CDC buried and twisted this fact that undermines their central claim.
The CDC makes it very difficult for readers to notice how they distort these studies. They do this by using unclickable footnotes and failing to link to the vast majority of the sources they cite. Thus, readers must note the footnote numbers, scroll down to the bottom of the webpage to locate the source, conduct a separate search for the source, and then scroll back up to the location where they were reading. Compare that runaround to a typical academic journal, where all of this can be done with a few simple clicks.
The CDC’s “Science Brief” on cloth masks is similarly deceitful. It makes its sources inaccessible, distorts the lone RCT on cloth masks, and ignores observational studies that don’t fit the narrative. Perhaps worst of all, it cites more than a dozen observational studies without ever revealing their fatal flaw: an inability to determine the actual effects of masks.
In contrast, the government health agencies of other nations, like Public Health England, are forthright about that reality and bluntly state that observational studies on masks are “highly subject to confounders,” and thus, they constitute “weak evidence.”
The CDC’s record of double-talk, double-standards, and outright falsehoods about masks should give pause to anyone who would blindly trust their pronouncements. Yet, tech giants like Google/YouTube and Facebook promote the CDC’s claims as unquestionable and censor people who challenge them.
Laboratory/Simulation Studies
When assessing the effects of masks and other medical interventions, the weakest form of evidence is laboratory/simulation studies. The World Health Organization, other public health agencies, and medical journals emphasize that such studies should “not directly inform policy decisions” because they are highly uncertain. In the words of Public Health England, this is because they:
- “provide only theoretical evidence.”
- “are run in controlled environments that may not accurately reflect the behaviours that we observe in real life.”
- “only provide mechanistic evidence which should be considered with caution.”
Despite providing flimsy clinical evidence, the facts surrounding these studies reveal strong evidence about how false beliefs about masks took root and the deadly consequences of those dogmas.
First, it is critical to understand how respiratory viruses spread because this is at the core of the issue. A 2021 paper in the journal Nature describes four primary ways in which such diseases can be transmitted:
- Direct physical contact when people touch one another.
- Indirect physical contact when people touch, sneeze, or cough on objects that are later touched by other people who then touch their mouth, nose, or eyes.
- Large respiratory droplets generated by talking, coughing, and sneezing that can travel through the air between people but are too heavy to stay airborne for more than a few seconds.
- Microscopic respiratory vapors (also called “airborne particles” or “aerosols”) generated by breathing, talking, coughing, and sneezing that are light enough to stay airborne for more than a few seconds.
If a disease is mainly spread by the second and third of those mechanisms, masks of all types can be helpful because they block large droplets created by coughing, sneezing, and “say it don’t spray it” talking.
But if a disease is mainly spread by the fourth and final mechanism, wide-ranging medical sources are clear that surgical and cloth masks are practically useless. This is because the pore sizes of these materials are not small enough—and the fit of such masks are not tight enough—to effectively block the spread of microscopic aerosols:
- A study published in 2003 by the Journal of Textile and Apparel, Technology, and Management analyzed six different types of surgical masks and found that their average pore sizes ranged from 17 to 51 microns, and their max pore sizes ranged from 27 to 147 microns. Collectively, these pore sizes are:
- 85 to 1,500 times larger than coronavirus virions, which are about 100–200 nanometers (0.1 to 0.2 microns) in diameter, including their spikes.
- at least 17 to 147 times larger than the vast bulk of virus-carrying aerosols exhaled by primates infected with C-19, more than 90% of which are less than 1 micron.
- The FDA’s Covid-19 guidance for surgical masks states that they cannot be labeled “for antimicrobial or antiviral protection” and cannot make “filtration claims” for particles of any size.
- A 2009 paper in the Journal of the International Society for Respiratory Protection documents that the “use of surgical masks will not provide respiratory protection against airborne virus particles expelled by humans during talking, coughing, breathing or sneezing.”
- A 2009 paper in the Journal of the Royal Society Interface reports that “aerosolized particles would readily penetrate or circumvent ordinary surgical masks.”
- A 2012 paper in the journal Respiratory Physiology & Neurobiology reported the results of an OSHA test which found that the ratio of particles outside a surgical mask to inside of it was 3.6—while N95 masks must have a ratio of at least 100:1 to meet OSHA’s standard. These facts were locked behind a paywall and buried 2,000+ words into the paper near the end of a 200+ word paragraph. The lead author of the paper was a CDC scientist.
- A 2013 paper in the Journal of Occupational and Environmental Hygiene explains that surgical masks have “poor filtration” and a “poor fit,” and thus, they “cannot be expected to significantly reduce the inhalation of infectious aerosols.”
- A 2013 paper in the AORN Journal explains that “surgical masks are intended for use as a barrier to protect the wearer’s face from large droplets and splashes of blood and other body fluids; however, surgical and high-filtration surgical laser masks do not provide enough protection to be considered respiratory PPE.”
- A study published in 2019 by the Annals of Translational Medicine found that the average pore size of a double-layer surgical mask is about 60 microns. This is at least 60 times larger than the vast bulk of virus-carrying aerosols exhaled by primates infected with C-19, more than 90% of which are less than 1 micron.
- A 2020 commentary in the Journal of the American Medical Association explains that if the virus that causes C-19 “is carried by aerosols that can remain suspended in the air for prolonged periods,” surgical masks provide “inadequate” protection because “aerosols can both penetrate and circumnavigate” them.
- A lab study published in 2020 by the journal Nature Medicine reports: “Our findings indicate that surgical masks can efficaciously reduce the emission of influenza virus particles into the environment in respiratory droplets, but not in aerosols.”
- A lab study published in 2021 by the journal Physics of Fluids tested the ability of common masks to filter aerosols of varying sizes expelled at a pressure equivalent to “normal breathing.” This is much easier than filtering higher pressure aerosols from “sneezing, coughing, laughing, and speaking.” Based on tests with the masks strapped to a mannequin, the study found that:
- all of the masks reduced “the forward momentum” of the aerosol stream, but “a significant fraction of aerosol escapes the masks, particularly at the bridge of the nose.”
- “in a relatively large indoor environment” and at “the widely accepted social distancing” separation of 6 feet, the aerosol levels compared to wearing no mask for 10 hours were reduced by 60% for an N95 mask, 46% for a KN95 mask, 46% for an R95 mask, 20% for an N95 mask with a one-way valve, 12% for a surgical mask, 10% for a cloth mask, and 3% for a loose-fitting N95.
- adding some air circulation to the room at a “relatively low” rate of two air exchanges per hour decreased the aerosol levels by more than any of the masks.
- The FDA states: “While a surgical mask may be effective in blocking splashes and large-particle droplets, a face mask, by design, does not filter or block very small particles in the air that may be transmitted by coughs, sneezes, or certain medical procedures.”
The facts above apply even more so to cloth masks, most of which have much worse filtration than surgical masks:
- A lab study published in 2019 by the journal PeerJ analyzed 20 different types of cloth masks and found that their pore sizes ranged from 80 to 500 microns. This is at least 80 to 500 times larger than the vast bulk virus-carrying aerosols exhaled by primates infected with C-19, more than 90% of which are less than 1 micron.
- A lab study published in 2010 by the Annals of Occupational Hygiene tested the permeability of “five major categories of fabric materials” to “the size ranges of virus-containing particles in exhaled breath.” Using a government “respirator test protocol” that specifies a mixture of particles below 1 micron, the study found that:
- these fabrics, “including sweatshirts, T-shirts, towels, scarves, and cloth masks” had “40-90% instantaneous penetration levels.”
- the three different types of cloth masks had penetration levels ranging from 74% to 90%.
- “face seal leakage”—which “is a critical component of respiratory protection” that “was not measured” in this study—will “further decrease the respiratory protection” of the masks and other fabrics.
- The 2015 paper that presented the RCT on cloth masks also reported the results of a lab study on them. Using a government “respiratory standard” that specifies a mix of particle sizes to be sprayed at masks at a certain flow rate, the study found that 97% of all particles passed right through the cloth masks, as compared to 44% for surgical masks. In the words of the authors, the study showed that:
- “filtration was extremely poor (almost 0%) for the cloth masks.”
- filtration was “poor” for the surgical masks, which makes it “unlikely” that they work very well, “particularly given that the predominant pathogen was rhinovirus, which spreads by the airborne route.”
Returning to the issue of whether Covid-19 is transmitted by aerosols, big tech’s chosen medical authorities butchered the pivotal facts of the matter. For a prime example, the World Health Organization published a “fact check” in March 2020 insisting that “Covid-19 is NOT airborne” and “is mainly transmitted through droplets” that “are too heavy to hang in the air”:
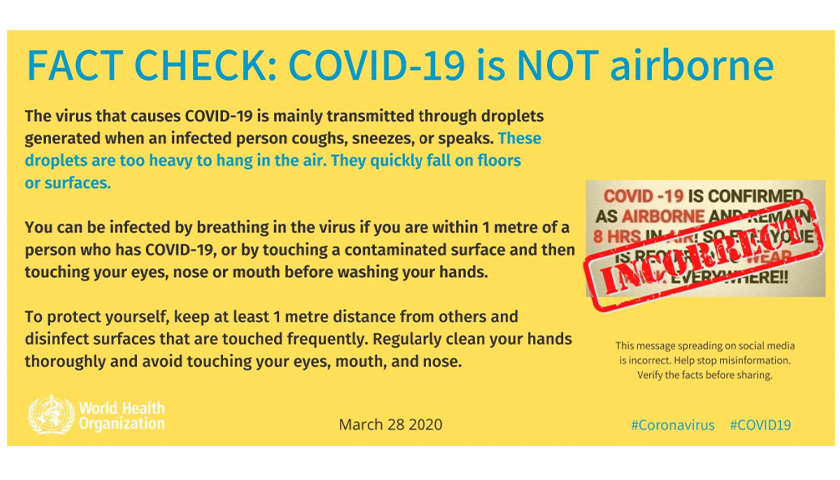 Similar claims about “droplets” were widely propagated by the likes of the CDC, Holmes Lybrand of CNN, and Paul Krugman of the New York Times.
Similar claims about “droplets” were widely propagated by the likes of the CDC, Holmes Lybrand of CNN, and Paul Krugman of the New York Times.
Exposing the hollowness, prevalence, and deadly potential of such claims, 14 authors of a June 2020 paper in the journal Environment International:
- analyzed multiple streams of evidence that are “strongly indicative of aerosols as one of several routes of Covid-19 transmission.”
- explained that “equivalent evidence for contact and large droplet transmission is not available” but has merely “been an unproven assumption from the outset.”
- lamented that “no countries or authorities consider airborne spread of Covid-19 in their regulations to prevent infections transmission indoors.”
- warned that aerosols “can result in large clusters of infection in a short period.”
- emphasized that “this failure to immediately recognize and acknowledge the importance of airborne transmission and to take adequate actions against it will result in additional” C-19 infections.
Six months later in November 2020, the journal Clinical Infectious Diseases published a statement signed by 239 scientists documenting “more than enough supporting evidence” that C-19 could be spreading via aerosols. These scientists also:
- stressed that “most public health organizations, including the World Health Organization,” have not come to grips with these facts.
- appealed to “the medical community and to the relevant national and international bodies to recognize” this reality and take measures to deal with it.
The failure of certain government agencies and media outlets to embrace those facts is not a case of “science evolving.” A wealth of studies have shown all along that aerosols play a dominant role in the transmission of all infectious respiratory microbes, including the one that causes C-19. In contrast, there is no such evidence for droplets or indirect contact:
- A study of microbes in operating rooms published by the journal Clinical Orthopaedics and Related Research in 1975 found that:
- the number of microbe colonies “jumped dramatically” (by 34 times) when people wearing surgical masks entered empty operating rooms, and the count of microbes “was no different than” when everyone in the room didn’t wear masks.
- the only way to explain these results is if microbes escape “out of the sides” of face masks or penetrate through them, which can only happen if they are transported by aerosols.
- A similar study published by the same journal in 1999 found that regardless of whether everyone or no one wore surgical masks in an operating room and in the hallway outside of it, there was “no effect on the bacterial counts in either the hallway or the operating room.” Again, this is only possible with aerosols.
- For a study published by the Journal of Infectious Diseases in 1987, researchers deliberately infected some of the subjects with a common cold virus, quarantined them for a few days, and then had them play a series of 12-hour poker games. Each of the games was played under unique conditions that would allow some modes of virus transmission while excluding others. For instance, the players wore a device during one of the games that made it physically impossible for them to touch their faces. The study found that “contrary to current opinion,” the cold virus is transmitted “chiefly by the aerosol route.”
- A 2004 paper in the New England Journal of Medicine proves that the only plausible explanation for “a large community outbreak of SARS in Hong Kong” was “virus-laden aerosols.”
- A 2009 paper in the Journal of the Royal Society Interface documents that:
- “increasing evidences point towards a role for aerosol transmission in the spread of influenza,” particularly “over short distance where exposure to both aerosol and large droplets occurs.”
- “a rigorous mathematical analysis of transmission by hand-to-face contact suggests that it plays but a minor role.”
- A study of flu infections published by the Proceedings of the National Academy of Sciences in 2018 found “overwhelming evidence that humans generate infectious aerosols” that are “small enough to remain suspended in air and present a risk for airborne transmission.” The study also found that 76% of aerosol particles smaller than 5 microns contained flu RNA, while only 40% of aerosols larger than 5 microns did so.
- A 2020 paper in the journal Risk Analysis reviews “three lines of evidence” on infectious disease transmission and concludes they warrant “urgent attention” because they show that “aerosol transmission is an important pathway of disease communication and may be significant for the transmission and control” of Covid-19.
- A 2020 paper in the Journal of Infectious Diseases confesses that the “modes of transmission” for C-19 are “not established” but are just “presumed to be mainly respiratory droplets and spread via fomites” (a term denoting indirect physical contact).
- A study published in 2020 by the journal Indoor Air documents that 53 of 61 attendees at a choir practice were likely infected by a single person who never got close to most of the others or touched anything that they touched. This rules out fomite or droplet transmission and implicates aerosols.
- A mathematical modeling study published in 2020 by the journal Building and Environment reports that:
- people have “commonly believed” since the early 1900s that large droplets are the “dominant” way in which respiratory infections spread, but that mechanism “remains surprisingly unexplored.”
- “the literature on large droplet transmission” provides “no direct evidence for large droplets as the route of transmission of any disease.”
- when compared to the “worst scenario in terms of large droplet transmission,” the airborne mode is “dominant,” even for coughing at close distances.
- “conventional surgical masks are not effective” at preventing airborne transmission.
- A study published by the Proceedings of the National Academy of Sciences in 2021 found that:
- the “majority of particles exhaled” by humans and primates are “small respiratory droplets” that “transmit through conventional masks and traverse distances far exceeding the conventional social distance of 2 m.”
- these “exhaled aerosol particles” dramatically increase with age, body-mass index, and the severity of C-19 infections.
- a “critical factor” in C-19 “superspreading” and “other transmission events is the propensity of certain individuals to exhale large numbers” of these aerosol particles.
- A 2021 paper in the Annals of Internal Medicine documents “a large cluster” of C-19 infections among staff and patients in a Boston hospital “despite a mature infection control program that included policies” like “universal masking of providers” and placing C-19 patients “in specialized units.” The authors thus conclude that these infections may be due to “aerosol transmission.”
- A study published by the International Journal of Infectious Diseases in 2021 proves that C-19 was transmitted via the air ducts of an apartment building, which is only possible via fine aerosols that remain airborne. This finding led the authors to conclude: “Our study implies that indoor infection risks through aerosols are underappreciated and urgently need attention.”
- A lab study published by the journal Anesthesia in 2021 found that:
- more than 92% of respiratory particles produced by breathing, talking, exercising and coughing were tiny aerosols that are 5 microns (0.0002 inches) or less.
- other lab studies that found fewer aerosols used inferior procedures like a “small sampling inlet” and “very low air sampling rates.”
- “when a surgical mask was worn, the apparent filtration increased” during most activities, but “this was partly due to masks deflecting gas away from” the measuring instrument and “backwards across” people’s faces, which “may blunt the forward plume and remove large droplets” but could still allow aerosols “to accumulate in poorly ventilated spaces.”
- aerosols “present a high risk of SARS-CoV-2 transmission,” and “the risk of aerosol exposure is underappreciated and warrants widespread, targeted interventions.”
After the publication of nearly all of those journal papers—plus others with similar findings like this, this, this, this, this, and this, and this—the World Health Organization and CDC nonchalantly walked back their longstanding and lethally false assertions about droplets and aerosols:
- On April 30, 2021, the World Health Organization changed its webpage on how Covid-19 is transmitted by:
- deleting this claim: “Current evidence suggests that the main way the virus spreads is by respiratory droplets among people who are in close contact with each other.”
- adding this statement: “A person can be infected when aerosols or droplets containing the virus are inhaled or come directly into contact with the eyes, nose, or mouth.”
- A week later on May 7, 2021, the CDC changed its webpage on “How COVID-19 Spreads“ by:
- deleting this claim: Covid-19 “infections occur mainly through exposure to respiratory droplets when a person is in close contact with someone who has Covid-19.”
- adding this statement: “Covid-19 spreads when an infected person breathes out droplets and very small particles that contain the virus.”
Instead of candidly announcing that they were wrong about this life-or-death issue, WHO and the CDC made those changes without fanfare.
Moreover, the CDC made a blatant attempt to cover its tracks. On the same day that the CDC changed its webpage on “How COVID-19 Spreads,” it created a “Scientific Brief” titled “SARS-CoV-2 Transmission“ that claims, “Although how we understand transmission occurs has shifted, the ways to prevent infection with this virus have not.” In reality, the implications of this shift are staggering:
- When the CDC deleted its claim that “airborne transmission” rarely occurs, it also deleted this incriminating fact: “Pathogens that are spread easily through airborne transmission require the use of special engineering controls to prevent infections,” including highly ventilated rooms and fit-tested respirators. This reveals that the CDC endangered healthcare workers and hospital patients by calling for such protections only when workers were involved in special “aerosol-generating” procedures like intubation and open suctioning. While operating under the CDC’s guidance that did not adequately protect people from aerosols, front-line healthcare workers became infected with C-19 at roughly 3.4 times the rate of the general population. This occurred even though the CDC recommended masks for healthcare workers since the outset of the C-19 pandemic under the false premise that droplets were the main cause of transmission.
- Mary-Louise McLaws, an epidemiologist and member of WHO’s Covid-19 infection control committee, told the New York Times in July 2020 that she was “frustrated” by WHO’s stubbornness on the issue of aerosols, wanted them to revisit this issue, and emphasized that a change in WHO’s position “will cause an enormous shudder through the infection control society” and that “we would have to be prepared to change a lot of what we do.”
- The reality that Covid-19 spreads mainly via aerosols adds to the body of evidence that certain governors turned nursing homes into death traps by forcing them to admit people with Covid-19. This is because aerosol-transmitted diseases like C-19 can spread like wildfire in nursing homes without specialized air disinfection systems, and most U.S. nursing homes don’t have them. Among the governors who issued such orders are Andrew Cuomo (D–NY), Phil Murphy (D–NJ), Tom Wolf (D–PA), Gretchen Whitmer (D–MI), and Gavin Newsom (D–CA).
- As detailed in a 2018 paper published by the Journal of Thoracic Disease, “outdoor air” ventilation “can effectively reduce the risk of long-range airborne transmission, while it may be of little use in preventing the droplet-borne transmission.” This is because aerosols accumulate indoors but disperse outdoors, while droplets quickly fall to the ground regardless of whether people are outdoors or indoors. This means that the government officials who issued lockdown orders that forced city residents to stay inside by closing all outdoor public areas intensified the C-19 death toll. To wit, NY Governor Andrew Cuomo (D) said during a May 2020 press conference that he found it “shocking” to discover that 66% of all people hospitalized for C-19 in NY had stayed home and rarely went out. Failing to realize the import of that, he bragged that “everything is closed down” and showed the “shocking” data on a slide that orders people to “STAY HOME. STOP THE SPREAD. SAVE LIVES.”

The harm caused by such policies is vividly illustrated by a recent New York Times article about nursing home residents who were “trapped indoors under lockdown” orders for nearly a year in Toronto, Canada (“the lockdown capital of North America”). Under government orders, the home forbid residents from leaving their buildings for “even a stroll” during “all but five weeks between March 2020 and June 2021.” Yet, the facility suffered a C-19 outbreak in which 35 staff and 53 residents tested positive, four of whom died.
Beyond the physical, cognitive, and emotional toll of isolating people and locking them indoors for a year, those strict nursing home lockdowns confined residents to indoor areas where aerosols are more likely to spread. Thus, 31% of Canadian nursing homes had C-19 infections among their residents or staff, and 31% of these led to outbreaks of 25 or more cases. As a result, about 80,000 residents were infected, and more than 14,000 of them died. Much of this could have been avoided if government mandates reflected the reality that C-19 is primarily transmitted by aerosols instead of droplets.
Given the abundance of evidence that is how C-19 spreads, and the lethal consequences of failing to recognize it, how could so many government agencies deny this reality for so long? They embraced a naive assumption that diseases commonly transmitted over short distances must be spread by droplets instead of aerosols—even though scientific journals explicitly debunked this fallacy:
- A 2009 paper in the Journal of the Royal Society Interface explains that “the demonstration of long-range infection implies aerosol transmission,” but “the converse, however, is not necessarily true.” This is because “aerosol particles are rapidly diluted, and are removed by ventilation,” which reduces the probability of long-range transmission.
- A 2020 paper in the journal Building and Environment found that when people are in “close contact,” the “airborne” mode of transmission “dominates” because droplets fall to the ground too quickly “to be deposited on the lip/eye/nostril mucosa” of other people unless they are “in very close contact.” By “very close,” they mean “0.2 m (8 inches) while talking or 0.5 m (1.6 feet) while coughing.” In plain words, you’d need to be an extremely close talker or cough right in people’s faces to transmit C-19 via droplets. Such behaviors are abnormal, especially during a pandemic.
- A 2021 paper in the journal Nature addresses the fatal flaw of a WHO scientific brief on C-19 transmission by documenting that “a failure to observe long-range transmission” is “not evidence against aerosol transmission.” This is because:
- “the observation that influenza virus viral load in aerosols decreased substantially with increasing distance from the source” suggests “that if aerosol transmission does occur, it will occur mostly at close range and rarely at long range.”
- “transmission via the droplet route in the absence of all other routes has yet to be observed” for any type of respiratory virus.
Even though the CDC has slyly admitted the truth about aerosols, it continues to overlook the threat in ways that can cause harm. Illustrating the depths of the CDC’s real or feigned blindness, it published a study on August 27, 2021 that:
- describes a C-19 outbreak involving an unvaccinated California elementary school teacher who worked for three days with a symptomatic case of C-19 and probably transmitted it to half of the students in his/her classroom.
- claims the outbreak proves the need for masking because “the teacher was reportedly unmasked on occasions when reading aloud in class.”
- reveals that “adherence to masking” among the students in the class was “high.”
- shows a seating chart displaying the teacher’s desk in a corner of the room and well over 50 feet between the teacher and the furthest student who likely caught C-19 directly from the teacher.
- does not even mention the topic of aerosols.
Unrealistic Lab/Simulation Studies
Despite the multitude of lab studies indicating that surgical and cloth masks are practically useless at reducing disease transmission by airborne viruses, the CDC insists that such studies show just the opposite. They do this by ignoring the more lifelike studies detailed above while cherry picking and misrepresenting unrealistic studies that:
- fail to measure the vast majority of aerosols that penetrate cloth and surgical masks.
- ignore all of the virus-laden particles that leak from the sides, top, and bottom of masks, which is a common weakness of surgical and cloth masks.
- are conducted during brief timeframes that don’t measure what happens after people breathe into a mask for more than an hour and saturate it with respiratory vapors.
- don’t account for the reality that cloth masks must be washed, and this increases their permeability.
- don’t account for the fact that cloth masks are often designed to be stretched across people’s faces in order to reduce the gaps around their edges, and this increases their permeability.
- don’t measure the infectious particles that are released into the air when people take off masks that have been harboring viruses in a warm, moist dark environment for hours.
For example, the anonymous authors of the CDC’s “Science Brief” on cloth masks cite two studies to support their claim that “multi-layer cloth masks” can “block up to 50–70%” of “fine droplets and particles (also often referred to as aerosols) smaller than 10 microns.” Neither of these studies come anywhere close to reflecting real-world circumstances.
The first of them, published in 2020 by the journal Aerosol Science and Technology, was a lab “simulation” of “a single cough” in “two consecutive tests.” It found that a 3-ply cotton cloth mask blocked 51% of aerosol particles smaller than 7 microns and 28% of particles smaller than 0.6 microns. Unlike the “50–70%” blockage rate claimed by the CDC, the 28% figure is more relevant to C-19 since greater than 90% of all virus-carrying aerosols exhaled by primates infected with C-19 are less than 1 micron.
Most importantly, the study mimics wearing a brand new face mask for a few seconds and fails to account for the following realities that other studies have addressed:
- A study published in 1975 by the British Journal of Surgery required people to wear each mask for 30 minutes before testing began “so that the masks would be already moistened and contaminated with organisms.”
- A study published in 2013 by the International Journal of Infection Control found that surgical and cloth masks “significantly decreased bacterial dispersal initially but became almost ineffective after two hours of use.”
- A study published in 2020 by the journal Nature found that the highest concentrations of C-19 aerosols in various areas of two hospitals were located in the rooms where healthcare workers removed their protective apparel (like masks). Thus, “virus-laden aerosols” are likely emitted “from the surface of the protective apparel worn by medical staff while they are removing the equipment.”
- A study published by The Lancet in 2020 tested the “stability” of the virus that causes C-19 on different surfaces at room temperature. Among the items tested (like paper, cloth, wood, and plastic), the one on which the virus survives the longest is a surgical mask. In the words of the authors, “Strikingly, a detectable level of infectious virus could still be present on the outer layer of a surgical mask on day 7,” about 0.1% of the initial virus.
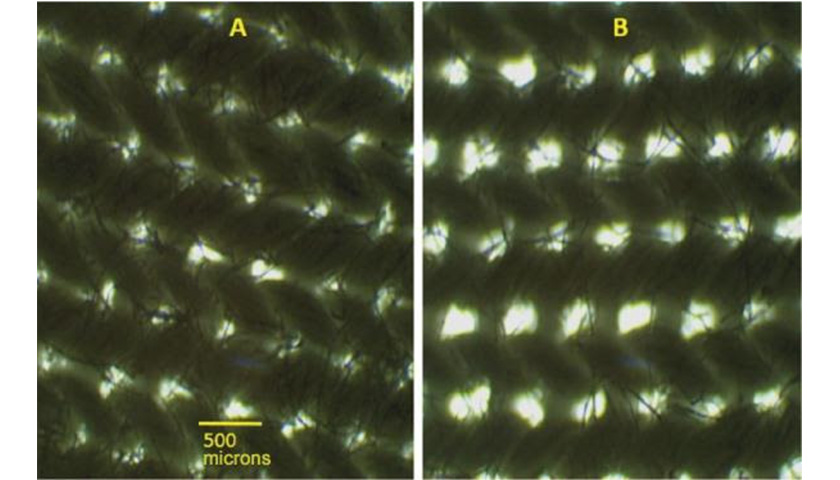
- A study published in 2019 by the journal PeerJ found that the filtering efficiency of cloth face masks “dropped by 20% after the 4th washing and drying cycle.” It also found that the act of stretching a cloth mask—which is often done to reduce the gaps around its edges—causes “an increase in pore size,” as shown on the right side of this picture:
The other study cited by the CDC was published by the journal mSphere in 2020. This study is more realistic than the first because it was conducted over 20 minutes instead of a few seconds, but this is still well short of the length of a school day or hospital shift. Nor does the study account for:
- the infectious aerosols that are released when people remove masks that have been incubating viruses in a moist, warm, and dark environment for hours.
- the degradation in mask performance caused by washing.
Another major flaw of the study is that the average size of the aerosol particles generated for the experiment was 5 microns. Again, more than 90% of particles exhaled by primates infected with Covid-19 are less than 1 micron. The study’s authors note that “some” of the larger “droplets likely gradually evaporated and changed to aerosols,” but this does not change the fact that the starting sizes of the particles in the experiment are much larger than the starting sizes of real-world C-19 particles.
The CDC’s “Science Brief” also cites four studies to weave a tale that cloth masks “limit the forward spread” of aerosols “that are not captured.” Yet, one of those same studies destroyed the CDC’s narrative when it found that surgical and cloth masks “generate significant backward leakage jets that have the potential to disperse virus-laden fluid particles by several meters.” Thus, the study concludes that:
the effectiveness of the masks should mostly be considered based on the generation of secondary jets rather than on the ability to mitigate the front throughflow.
And yet again, the CDC makes it hard for readers to discover these vital facts by using unclickable footnotes and not linking to the study.
Also, the CDC’s 4,000+ word “Science Brief” on cloth masks does not contain the word “leak” or any synonym for it. The deceitfulness of that omission is underscored by a 2010 paper in the Annals of Occupational Hygiene which emphasizes that “face seal leakage of aerosol particles” is “a critical component of respiratory protection.”
In sum, a torrent of facts related to lab studies prove that the CDC, WHO, and other agencies that were formed to protect people’s health:
- told the general public to wear cloth masks based on the false assumption that Covid-19 is mainly spread by large droplets that are blocked by such masks.
- disregarded reams of studies that showed Covid-19 is mainly spread by aerosols that are less than 1/80th the size of the pores in the finest cloth masks.
- used the same false assumption about large droplets to create hospital and nursing home guidance that discounted the threat of aerosols and thereby killed untold numbers of people.
- quietly walked back that assumption in the spring of 2021 while deleting a statement that exposes the harm that it caused.
- misconstrued and cherry-picked unrealistic studies to claim that cloth masks protect people from aerosols while ignoring far more realistic studies that show otherwise.
- have still not updated their hospital and nursing home guidance to properly protect against aerosol transmission, thus allowing countless preventable deaths to continue.
Throughout all of this, massive corporations like Google/YouTube and Facebook helped spread these deadly fictions.
Asymptomatic/Presymptomatic Transmission
Another misleading aspect of the CDC’s case for masks is the claim that people with asymptomatic and presymptomatic C-19 can easily transmit the disease.
The first paragraph of the CDC’s “Science Brief” on cloth masks declares that masks are “especially relevant for asymptomatic or presymptomatic infected wearers who feel well and may be unaware of their infectiousness to others, and who are estimated to account for more than 50% of transmissions.” The facts, however, show that claim has no basis in reality:
- A 2020 paper in the journal Nature Medicine documents that fears about widespread transmission of C-19 by asymptomatic and pre-symptomatic people stemmed from models, and real-world observations from “direct contact tracing studies” have proven that the actual threat is “lower than that predicted by Covid-19 transmission models.”
- A contact tracing study published by the Annals of Internal Medicine in 2020 found that merely 1 among 342 people who had “close contact” with asymptomatic C-19 virus carriers caught the disease from them.
- A meta-analysis published by the journal JAMA Network Open in 2020 found that less than 1% of people with asymptomatic or pre-symptomatic Covid-19 infect other members of their households. These results led the authors to remark that “the lack of substantial transmission from observed asymptomatic index cases is notable.”
So how can the CDC claim just the opposite? By citing two studies that use speculative models, while ignoring every study that uses real-world data. Both of the studies cited by the CDC state that they are based on a “model,” and the second one is explicit that the model uses the “assumption” that asymptomatic people “are 75% as infectious as those who do develop symptoms.”
In other words, the CDC cherry picks studies that rely on an assumption that the CDC misrepresents as a fact. And once again, the CDC makes it hard for readers to discover this by using unclickable footnotes and not linking to the studies.
The Harms of Masks
Facebook has enacted a policy to censor “false health information” that is “widely debunked by leading health organizations such as the World Health Organization and the Centers for Disease Control and Prevention.” This includes any “claims that wearing a face mask can make the wearer sick.”
That policy is self-contradicting because the World Health Organization published “interim guidance“ on masks in 2020 that reveals exactly what Facebook bans everyone from saying. Per the guidance, “The likely disadvantages of the use of masks by healthy people in the general public include”:
- “potential increased risk of self-contamination due to the manipulation of a face mask and subsequently touching eyes with contaminated hands.”
- “potential self-contamination that can occur if non-medical masks are not changed when wet or soiled. This can create favorable conditions for microorganism to amplify.”
- “potential headache and/or breathing difficulties, depending on type of mask used.”
- “a false sense of security, leading to potentially lower adherence to other critical preventive measures such as physical distancing and hand hygiene.”
Reams of facts from science journals confirm those and other harms of surgical and cloth masks.
Headaches
A range of studies show that surgical and N95 masks induce headaches in some people.
In 2009, the American Journal of Infection Control published the results of a small RCT of surgical masks involving 32 healthcare workers for 77 consecutive days. It found that workers assigned to wear masks “were significantly more likely to experience headache” than the maskless group. On average, the daily headache rate for maskless workers was 1.3%, while it was 4.9% for mask wearers—a 3.8-fold increase.
Similarly, a study published in 2019 by the journal BMC Infectious Diseases found that 6% of hospital workers who wore a surgical mask for one shift reported a headache.
Because N95 masks have finer filters and tighter fits than surgical masks, they restrict breathing more heavily, cause greater facial pressure, and are more uncomfortable. As such, a study published in 2006 by the journal Acta Neurologica Scandinavica found that 37.3% of 212 frontline healthcare workers in a Chinese hospital “reported headaches when they wore the N95 face-mask.” Among the workers who experienced headaches, 62.7% “had no pre-existing headaches.”
Similarly, a study published in 2020 by the journal Headache evaluated 158 frontline healthcare workers in a Singapore hospital early during the C-19 pandemic and found that:
- 81.0% of them developed headaches when wearing personal protective equipment, which included N95 masks and eye protection.
- among the workers who had a pre-existing problem with headaches, 91.3% “agreed” or “strongly agreed” that “the increased PPE usage had affected the control of their background headaches, which affected their level of work performance.”
- among the workers who experienced headaches:
- 53.1% thought that the N95 mask was the “likely” cause of a headache.
- 81.3% developed a headache within 60 minutes of putting on the mask.
- 88% had a “headache resolved spontaneously” within 30 minutes of taking off the mask.
Breathing
Though far from universal, a substantial portion of people who wear masks report difficulty breathing:
- A study conducted in 14 Vietnamese hospitals and published in 2015 by the journal BMJ Open found that 18.3% of healthcare workers who wore a cloth or surgical mask reported “breathing problems.”
- A study published in 2019 by the journal BMC Infectious Diseases found that 12% of hospital workers who wore a surgical mask for one shift reported “breathing difficulty.”
- A study published in 2021 by the International Journal of Bioinformatics and Biomedical Engineering found that 22% of 183 medical students at a college in India “experienced breathing difficulty” while wearing N95, surgical, or cloth masks.
The studies above lay out several reasons why masks may cause headaches and problems with breathing, such as increased carbon dioxide, excessive heat, and facial pressure. These and other factors are explored next.
Carbon Dioxide
Because humans create carbon dioxide as they breathe, the CO2 concentration of the air they exhale (4% to 5%) is about 100 times higher than in fresh air (0.04%). Although CO2 is generally non-toxic, ingesting too much of any substance will cause harm. Thus, governments throughout the world set maximum indoor CO2 limits for homes, schools, submarines, and other places where CO2 can accumulate because fresh air does not flow freely.
Similarly, science journals have proven that face masks restrict airflow and cause the wearers to rebreathe some of the air they exhale. This raises the CO2 levels in the air they inhale to well above that of fresh air. These levels are far beyond government CO2 limits for schools and workplaces, and certain people have tried to bury these facts:
- A lab study published in 2013 by the Annals of Occupational Hygiene measured CO2 levels in the breathing zones of 30 different models of N95 masks. Ten pages deep into their paper, the authors reveal that the average CO2 concentrations ranged from 1.3% to 3.5%. These levels are:
- A lab study published in 2021 by the journal Aerosol and Air Quality Research measured CO2 levels in the breathing zones of a surgical mask and a 3-layer cloth mask while a 50-year-old male wore them. The study found that the average CO2 concentration in:
- the cloth mask was 2,051 parts per million (ppm)—or four times the 501 ppm level “when no mask was worn” and twice the 1,000 ppm classroom limit for CO2 in many countries.
- the surgical mask was slightly higher at 2,107 ppm, and this increased to 2,875 ppm when the subject walked on a treadmill at a moderate pace.
- both masks was in the “range” associated with the “health symptoms” of “sick building syndrome.”
- A lab study published in 2021 by the journal BMC Infectious Diseases measured the CO2 levels in four types of masks near the smile lines of 11 healthy volunteers aged 16 to 54 years. Regarding the design, results, and presentation of this study:
- In a KN95 mask, the average CO2 concentration was 24,000 ppm. This is 24 times the classroom limit for CO2 in many countries (1,000 ppm).
- A “KN95” is not the same as an “N95,” and the authors of the study failed to mention the difference between these similar-sounding masks. As documented by a 2021 paper in the journal PloS One, KN95 masks are certified under a “Chinese standard” and “failed to fit any participant adequately enough to offer protective benefits above what might be achieved by a surgical or fabric mask.”
- In a “valved respirator” mask, the average CO2 concentration was 26,000 ppm, or 26 times the classroom limit for CO2 in many countries (1,000 ppm).
- Valved masks, as explained in the journal Aerosol and Air Quality Research, are “not recommended as an effective barrier against the SARS-CoV-2 virus because the valve releases unfiltered air when the wearer breathes out and therefore does not prevent the wearer from spreading the virus.”
- The authors of the study—who claim that they selected certain masks “due to their ubiquity in healthcare practice”—did not present any results for an N95 mask, even though N95s are “widely used in healthcare to reduce transmission of airborne infectious diseases.” Nor did the corresponding author reply to an inquiry from Just Facts about why they excluded the N95.
- The authors of the study claim in their conclusion that the CO2 levels in the masks they tested “remain within” government “limits for short-term use,” and “therefore, there should not be a concern in their regular day-to-day use for healthcare providers.” However, healthcare workers often wear masks for much longer than the short-term limit, which is merely 15 minutes. For instance, a 2003 paper in the Journal of Emergency Nursing reported that nurses in a Toronto emergency room were “working 12-hour shifts with an N95 mask.” This is a clear concern for healthcare providers given that the CO2 levels in the tested masks were five times OSHA’s work shift limit, which is 5,000 ppm.
All of the studies above were conducted in well-ventilated labs with CO2 levels close to that of fresh air (400 ppm). In the real world, indoor CO2 levels are often much higher, and this may push the CO2 concentrations in the masks to well beyond what lab studies have found. For example, a 2017 paper in the journal Indoor Air summarizes the results of more than 25 CO2 studies in schools across the world as follows:
- “In all studies, the reported average and median values of the peak CO2 concentration exceeded 1,000 ppm, and in many instances 2,000 ppm was exceeded.”
- “Also, the maximum peak CO2 concentrations range from about 3,000 to 6,000 ppm.”
- “A majority of the averages and medians of time-average concentrations also exceeded 1,000 ppm with maximum values ranging from 1,400 ppm to 5,200 ppm.”
On the other hand, government exposure limits for CO2 and other substances typically include a margin of safety to address uncertainties and protect people with serious health problems. Thus, the CO2 levels measured in masks don’t necessarily cause harm just because they exceed government limits for workplaces and schools. That said, ample studies show that the CO2 levels in masks do cause harm, especially in N95s.
The 13,000 to 35,000 ppm CO2 concentrations in N95 masks and KN95 masks are in the range of the 28,000 ppm level found to cause chest pain and the 20,000 ppm level found to cause headaches in a range of studies summarized by a 2007 paper in the Proceedings Of The National Academy Of Sciences.
Far below those levels, the 2,000 to 2,900 ppm CO2 concentrations in surgical and cloth masks may impair certain high-level brain functions:
- A study of 22 people published in 2012 by the journal Environmental Health Perspectives found the following impacts from 2.5 hours of CO2 exposure at 2,500 ppm:
- “Large and statistically significant reductions” in 7 out of 9 categories of decision-making performance in a test of “real-world day-to-day challenges.” These included measures of initiative, information usage, strategic thinking, and other factors associated with life success.
- Losses in 5 categories of decision-making performance that sunk “to levels associated with marginal or dysfunctional performance.”
- A gain in one category of decision-making performance (focus), which is common among people who have “mild-to-moderate head injuries” or are “under the influence of alcohol.” This is because such events cause people “to become highly focused on smaller details at the expense of the big picture.”
- A study of 30 active commercial aircraft pilots published in 2018 by the journal Nature found the following impacts from CO2 exposure in a flight simulator at levels ranging from 700 to 2,500 ppm:
- As scored by FAA-Designated Pilot Examiners, the pilots’ odds of properly executing complex flight maneuvers significantly decreased at a CO2 level of 2,500 ppm.
- “Passing rates were twice as high at 700 ppm and 1500 ppm during a takeoff with an engine fire than at 2500 ppm, and four times as high at 700 ppm during a RTO [rejected takeoff] than at 2500 ppm.”
- “The effect of CO2 on passing rates became more pronounced the longer the pilots were in the simulator, with the dose–response between CO2 and passing rate becoming apparent after 40 min of exposure.” A dose–response effect, as explained by epidemiologist Sydney Pettygrove, “is one in which increasing levels of exposure are associated with either an increasing or a decreasing risk of the outcome.” When this pattern occurs, it “is considered strong evidence for a causal relationship between the exposure and the outcome.”
- Some examples of the pilots’ failures at 2,500 ppm included, “Did not deploy the reversers/did not call,” “No callout/ disconnected auto-brakes,” and “did not set parking brake.”
In contrast, a study published by the journal Indoor Air in 2017 found “no statistically significant effects” on the “cognitive performance” of 25 people exposed to 3,000 ppm of CO2 for 255 minutes. However, locked behind a $59 paywall, the paper reveals that there were significant effects on some measures of cognitive performance, even though none of the tests were very demanding:
- “Among the many tasks examining the impact of exposure conditions on the performance of subjects, there were only a few for which conditions had a significant effect on performance.” These included:
- the speed and the error rates during simple addition (adding “five two-digit numbers printed in the same vertical column”).
- redirection (looking at images of a person facing in different directions with object in his hand and correctly identifying whether he is holding the object in his left or right hand).
- number linking (tracing “a line as quickly and accurately as possible through a series of two-digit numbers scattered randomly over a page, essentially rank-ordering them in sequence”)
- The cognitive tests used for the study resembled “office work,” while other studies (including the ones above) used “more complex” tests that impose “considerable cognitive load” and require more brainpower.
While ignoring those genuine facts from science journals, Facebook’s “independent fact checkers” like PolitiFact have quoted the mere opinions of cherry-picked “experts” to claim that “using ordinary cloth or surgical masks poses little or no risk from CO2.” Facebook then uses such bogus “fact checks” to suppress actual facts and malign those who share them.
One of the most sophomoric arguments made by Facebook’s enforcers comes from a group called Health Feedback and is parroted by another such group called Lead Stories. They claim that “face mask filters are small enough to keep out infectious droplets containing viruses, but gas molecules such as carbon dioxide and oxygen can still pass through freely.” This is grossly misleading in two respects.
First, the issue is not if CO2 penetrates masks (it obviously does)—but if a significant amount of CO2 is reinhaled because it stays inside the masks between breaths. The facts are overwhelming that this is what happens:
- A computer simulation published by the journal Trauma and Emergency Care in 2016 modeled a 47-year-old female wearing an N95 mask and found that “60% of respired air reentered the nasal cavity during the consecutive respirational cycle.”
- A study published by the journal Anesthesia in 2006 measured CO2 levels in the air exhaled by people wearing an N95 mask and found that CO2 rose “due to rebreathing” of air “that is ‘trapped’ in the respirator, with the degree of rebreathing being proportional to the volume of the respirator (‘dead space’).”
- A computer simulation published by the journal Physics of Fluids in 2021 found that an N95 mask increases “CO2 inhalation by approximately 7× greater per breath compared with normal breathing” because the “mask restricts the ability of the exhaled air to mix with the ambient air, leading to an accumulation of CO2 inside the mask.”
Second, Facebook’s luminaries seem to be ignorant of the fact that C-19 spreads mainly through aerosols, not droplets. They don’t even seem to understand the difference between them, as evidenced by the following sentence where they treat the words as synonyms: “The purpose of these masks is to reduce contact with infectious droplets (aerosols), which can be generated by someone who coughs or sneezes, and thereby minimize the risk of infection transmission.”
Just Facts has communicated with Facebook about the simple-minded falsehoods spread by its so-called “independent third-party” fact checkers, and Facebook has repeatedly dodged these questions:
- Given that Facebook has hand-selected these organizations to be the judges of truth on your platform, do you hold them to actionable standards and count quality violations against them?
- If so, what exactly are these standards and the repercussions for violating them?
- If not, why are you vesting certain people with unchecked authority to use Facebook to censor others, sow misinformation, and slander the reputations of scholars.
Cardio-Pulmonary Stress
An array of science journals have published studies showing that exercising with a mask causes heart and lung stress, negatively impacts performance, and may have caused some deaths:
- A study published in 2020 by the journal Clinical Research in Cardiology measured effects of surgical and N95 masks on 12 healthy males aged 32 to 42 as they exercised vigorously. The “sample primarily consisted of physicians working at a university hospital who are very familiar with medical masks and have a positive attitude towards personal protection.” The study found that:
- “ventilation, cardiopulmonary exercise capacity and comfort are reduced by surgical masks and highly impaired by” N95 masks.
- the masks “have a marked negative impact on cardiopulmonary capacity that significantly impairs strenuous physical and occupational activities.”
- the masks also have “a significant impact on pulmonary parameters” when resting.
- the masks “significantly impair the quality of life of their wearer” by causing “breathing resistance, heat, tightness,” and “severe subjective discomfort during exercise.”
- A study published in 2020 by the Asia-Pacific Journal of Sports Medicine, Arthroscopy, Rehabilitation and Technology measured effects of wearing a surgical mask while exercising moderately. The sample consisted of 23 people aged 21–60 who walked on a treadmill for six minutes to simulate “outdoor recreational hiking on an uphill slope at a comfortable pace.” The study found that the mask:
- “significantly increased” their heart rates by an average of 4.4 beats per minute.
- “significantly increased” their rates of perceived exertion from an average of 10.8 to 12.7 on a 20-point scale.
- caused “higher physiological responses,” “possibly due to restricted ventilation, heavier breathing, and sympathetic responses.”
- caused “an uncomfortable feeling of dyspnoea [shortness of breath]” for “some volunteers.”
- increased “the physiological burden” on their bodies, “especially in those with multiple underlying comorbidities.”
- A 2020 paper in the journal Medical Hypotheses found:
- “Recently, there have been case reports of sudden cardiac death (SCD) occurring during exercise with facemasks.”
- Exercise “with facemasks may increase the risk of SCD via” several mechanisms detailed in the paper.
- We “advise avoidance of a facemask during high intensity exercise, or if wearing of a mask is mandatory, exercise intensity should remain low to avoid precipitation of lethal arrhythmias [heartbeat irregularities].”
- We “cannot exclude the possibility” of a fatal cardiac event caused by a mask during “low intensity exercise especially” for people with heart disease.
- A study published in 2021 by the journal Applied Sciences measured effects of a surgical mask on 72 recreational athletes as they ran at their maximum speed for 50 meters and 400 meters. The study found that the mask:
- “increased blood lactate concentration, sympathetic autonomic modulation, perceived exertion, perceived stress, and decreased blood oxygen saturation.”
- “negatively affected” their “running performance” by increasing the average time to complete a 50m race by 12.51% and a 400m race by 19.09%.
- A study published in 2021 by the British Journal of Sports Medicine measured effects of a cloth mask on 31 healthy adults aged 18–29 years as they ran at max speed on a treadmill. The study found that the mask:
- “led to a 14% reduction in exercise time.”
- reduced their “maximal oxygen consumption” by 29%.
- caused the participants to feel “increasingly short of breath and claustrophobic at higher exercise intensities.”
Continuing its pattern of deceit, the CDC’s “Science Brief” on cloth masks ignores all of the studies above and cherry picks studies that use low exercise intensities, low exposure times, imprecise measurements, or gravely misleading summaries, like these:
- A study published in 2012 by the journal Respiratory Physiology & Neurobiology measured effects of a surgical mask on “young, healthy adults” while exercising. The sample consisted of 20 people (average age of 23 years) who walked on a treadmill for 60 minutes at a “low-moderate” pace of 3.5 miles per hour. Regarding the results of the study and the presentation of them:
- The mask increased the average heart rate of the participants from 117 to 128 beats per minute. For a frame of reference, an 11-point increase in heart rate is considered to be “a large change” in a study that examined the cardiac effects of certain drugs and “a large increase” in a study that examined the physiological effects of emotions.
- The mask “minimally increased” their respiratory rate by an average of 1.6 breaths per minute.
- The mask did not “significantly” increase their average core temperature.
- Behind a paywall, the paper reveals that 92% of the participants complained about some aspect of the mask.
- The lead author of the paper was a CDC scientist, and the authors titled it, “Absence of Consequential Changes in Physiological, Thermal and Subjective Responses From Wearing a Surgical Mask.”
- A study published in 2020 by the Journal of the American Medical Association measured effects of a disposable 3-layer face mask on 25 people aged 65 and older “while they were at rest or performing usual activities of daily living at home.” Regarding the methodology, results, and presentation of this study:
- The study found that wearing this brand of mask “was not associated with a decline in oxygen saturation in older participants.”
- The participants measured their own oxygen saturation levels using an over-the-counter pulse oximeter. Concerning these instruments, the FDA warns, “Do not rely only on a pulse oximeter to assess your health condition or oxygen level.”
- A study published in 2016 by the journal Anesthesia & Analgesia tested six over-the-counter pulse oximeters and found that their precision at normal blood oxygen levels varied from 0.88% to 1.81%. For a frame of reference, a 2008 paper in the journal Neurocirugia explains that a “very small” change in oxygen saturation of about 1.3% “reflects a large decrease” in the partial pressure of oxygen and “may have a clinical value for the health workers and the surgeons.”
- The authors report that they excluded from the study people with serious “cardiac or respiratory conditions” and “none of the participants’ SpO2 [oxygen saturation] fell below 92% while wearing masks.” Concerning these levels, the FDA states, “Oxygen saturation values are between 95% and 100% for most healthy individuals, but sometimes can be lower in people with lung problems.”
- A study published in 2021 by the Annals of the American Thoracic Society measured effects of a surgical mask on 15 healthy doctors (average age of 31) and 15 patients (average age of 72) with severe chronic obstructive pulmonary disease (COPD) as they rested and after they walked. Regarding the results of the study and the presentation of them:
- The study found “no major changes” of “clinical significance” in the oxygen saturation of the participants’ blood or the CO2 concentration of their exhaled breath when they wore a mask for 30 minutes while resting. Concerning this timeframe, a 2018 paper in the journal Nature documents that the physiological impacts of elevated CO2 on office workers and pilots don’t manifest until 40 to 60 minutes.
- The walking test for this study was conducted over six minutes and only on the COPD patients while they wore masks. The study did not establish a baseline for walking “without a mask” because “our institution” required everyone to wear masks in the room where the walking test was performed.
- The study found that the COPD patients “did not exhibit major physiologic changes” from walking with a mask “as a group.” Two of the patients, however, required “supplemental oxygen” during or after the walk, and the authors buried in a table the fact that one of the patients experienced a 19.0 percentage point drop in their oxygen saturation. Per the Center for Evidence-Based Medicine at Oxford University, “even a small” decline in oxygen saturation during “exercise should alert the clinician and a drop of 3% should be cause for serious concern, regardless of the amount of exercise needed to produce it.”
- The authors closed their paper by claiming, “It is important to inform the public that the discomfort associated with mask use should not lead to unsubstantiated safety concerns as this may attenuate the application of a practice proved to improve public health.”
In short, the CDC’s risk-free portrayal of exercising while masked is false and dangerous.
Furthermore, people who have acted in accord with the facts of this matter have paid a heavy price. A prime example is Bradley Keyes, a high school track and field coach who was fired by Pembroke Academy in New Hampshire for refusing to make his athletes wear masks.
Heat & Discomfort
The heat, humidity, and other discomforts of wearing a mask are not merely annoyances. This is because “heat and moisture trapping beneath surgical face masks,” as explained in the Journal of Hospital Infection, may cause “decreased mental and physical performance.”
Measured by the heat index, the interiors of masks can be sweltering, even in climate-controlled rooms. A study published in 2012 by the journal Respiratory Physiology & Neurobiology found that when “young, healthy adults” engaged in “low-moderate” intensity exercise with a surgical mask, the air inside the masks averaged 91°F (32.74°C) and 91% relative humidity. This equates to an heat index of 127°F (52.9°C). For comparison, the air in the room where the test was conducted was 71°F (21.47°C) and 23% relative humidity, a heat index of 69°F.
A study published in 2020 by the journal Clinical Research in Cardiology measured effects of surgical and N95 masks on 12 healthy males aged 32–42 as they exercised. It found that the masks “significantly impair the quality of life of their wearer” by causing “breathing resistance, heat, tightness,” and “severe subjective discomfort during exercise.”
A study conducted in 14 Vietnamese hospitals and published in 2015 by the journal BMJ Open found that 40.4% of healthcare workers who wore a cloth or surgical mask reported “adverse events associated with facemask use,” with “general discomfort” and “breathing problems” being “the most frequently reported adverse events.”
In 2021, the Journal of Transport & Health published a covert study of 182 passengers on subways and local trains in the area of Paris, France. It found that during a median observation time of 8 minutes, 48% of people touched their masks, and they did so at an average rate of 15 times per hour. The study also revealed an “increased tendency to touch the face while wearing a face mask” and noted that this “might increase the risk of transmission and self-contamination.”
The implications of mask touching are much broader than transmission and contamination. This is because momentary distractions (like adjusting a mask) can hamper job performance. A series of experiments published by the Journal of Experimental Psychology in 2008 found that “an entirely irrelevant distractor can interfere with task performance” by causing “increased error rates” and “response times.”
For people working in hospitals, factories, and offices where mental sharpness or attention to detail are vital to safety or performance, the discomforts and distractions of masks could make the difference between life and death. This is not a mere hypothetical because the fatal line can be easily crossed in certain environments. Based on a systematic literature review published by the Journal of Patient Safety in 2013, “there are at least 210,000 lethal” errors in U.S. hospitals each year, and “the true number” is “estimated at more than 400,000 per year.”
Social Bonds & Communication
Along with headaches, trouble breathing, cardio-pulmonary stress, discomfort, and cognitive impairment, another significant realm of harms caused by masks is relational:
- A study published in 1996 by the journal Perceptual and Motor Skills investigated how smiles—which are hidden by masks—affect people’s perceptions of other people. The study involved a sample of 330 Brazilian college students who were shown photos of people who were smiling and not smiling. Consistent with earlier research documented by the authors, the study found:
- “a powerful effect of facial expression on person perception.”
- smiling people were perceived as kinder, more attractive, more sympathetic, more sincere, more sociable, and more competent.
- As explained by a 2009 paper in the American Journal of Infection Control, people “cannot see most facial expressions of a person wearing a mask,” and this can impede social bonding “because it obscures an important nonverbal mode of communication.”
- A study published in 2008 by the journal Neuropsychologia evaluated the memory and brain activity of 18 young adults who were shown pictures and names of people with smiling and neutral faces. The study found that:
- the subjects remembered the names of 59.0% of the smiling faces and 46.8% of the neutral faces.
- the smiling faces activated certain regions of the subjects’ brains more fully than the neutral faces.
- “rewarding social signals from a smiling face” can enhance “relational memory.”
- In 2020, a trade journal called the Hearing Review published a lab study of communication impediments caused by N95 and surgical masks. The study and other research conducted by the authors showed the following:
- A “cornerstone of patient safety and quality healthcare is effective communication which allows patients to participate fully in their care.”
- Healthcare is “often being delivered in settings which are extremely noisy and distracting—replete with alarms beeping and ongoing competing conversations between patients and providers.”
- “Our findings were not unexpected but were unsettling.” Masks filtered out “the high frequencies (2000–7000 Hz) spoken by the wearer, with the decibel (dB) level of attenuation ranging from 3 to 4 dB for a simple medical mask and close to 12 dB for the N95 masks.” For reference, a reduction of 10 dBs amounts to halving the loudness of sound.
- “In short, the speech quality degradation, in combination with room noise/reverberation and the absence of visual cues, renders speech close to unintelligible for many.”
- A study published in 2020 by the Journal of Laryngology & Otology found the following about communication impediments caused by using N95 surgical masks with face shields:
- “Use of personal protective equipment [PPE] significantly impairs speech perception.”
- The volume at which people could recognize certain two-syllable words spoken by someone wearing an N95 mask and a face shield must increase by 12.4 decibels to be equivalent to someone speaking without PPE. This amounts to a doubling in loudness.
- Even at 40 decibels above the speech reception threshold, the ability of people to recognize certain words spoken by someone wearing an N95 mask and a face shield declined by 7%.
- “Our study was performed in a sound-treated audiology setting in order to standardize the environment for quantitative assessment. However, most conversations in the healthcare setting occur in the scenario of significant ambient noise. This may further impair speech perception and intelligibility.”
- “The role of cues obtained from lip reading and facial expressions in the perception of speech cannot be ignored. These might have a negligible role in a normal hearing individual and in a quiet environment, but not for those with hearing impairment and in the presence of background noise.”
- A study published in 2021 by the journal Frontiers in Psychology measured the ability of 119 people to sense the emotions of people who were masked. The study and other research conducted by the authors showed that:
- “facial movements and situational cues are crucial when interacting with others.”
- “a mask obstructing a face limits the ability of people of all ages to infer emotions expressed by facial features.”
- “the difficulties associated with the mask’s use are significantly pronounced in children aged between 3 and 5 years old.”
- “sensitivity to facial emotion movements is fundamental to children’s emotional processing and social competence.”
- “early childhood is considered a critical period for the development of understanding emotions and emotion processing,” and “young children’s future social abilities should be monitored to assess the true impact of the use of masks.”
Human beings, and especially youth, are highly social creatures. Masks stifle that by interfering with bonding and communication, which are essential to people’s mental health, physical health, and productivity.
Because association does not prove causation, it is impossible to empirically determine if widespread masking has played a role in the accompanying surges of depression and anxiety among youth, suicides among teens and young adults, and drug overdoses among people of all ages. But given the effects of masks on relationships, it would be mindless and irresponsible to ignore or dismiss this possibility.
Ultraviolent Air Disinfection
Beyond ordinary measures like social distancing, the risk of spreading diseases that are transmitted by aerosols can be greatly reduced by disinfecting air with ultraviolent (UV) light, an invisible part of the energy spectrum emitted by the sun. This simple and safe technology proficiently kills airborne microbes and has been successfully used to control the spread of contagious respiratory diseases for more than 80 years.
In 1942, the American Journal of Epidemiology published a series of experiments conducted at two Philadelphia-area schools with students from grades 1 to 12 during 1937–1941. The researchers installed UV lights to disinfect the air above students’ heads in some hallways, common rooms, and classrooms. This is called “upper room” UV.
The authors referred to these areas as “irradiated” even though “only indirect irradiation” was used in the classrooms. This was a vital aspect of the study design because it prevented the UV light from neutralizing microbes near the faces of the students or anywhere below them. Hence, the UV light could not prevent disease transmission via respiratory droplets or contact between the students or objects they touched. In other words, the experiments would only be successful if the diseases were mainly spread by aerosols.
The experiments were seemingly successful and found “no epidemic spread” of measles, chicken pox, or mumps “among the highly susceptible groups of children of the primary schools within irradiated atmospheres, although epidemic spread has occurred among less susceptible groups of older children in the departments of the schools whose atmospheres were not irradiated.” Put simply, students rarely transmitted these diseases to each other in areas with UV lights, while they often did so elsewhere.
The results included a period during “the largest epidemic of measles from which the city of Philadelphia has ever suffered.”
The study was not an RCT, so other factor(s) besides the UV lights could have been at play. However, the authors noted that “the patterns of the epidemics” in these “schools were strikingly different from any previous experience.”
Another limitation is that there were opportunities for students to mingle in areas that were not irradiated (like an auditorium) and outside of school. Hence, the studies found no change in the “total numbers of colds after installation of the lights,” which could be due to “home and random infections.” This kind of transmission is more likely with colds than measles, chicken pox, or mumps because “adults as well as children” often have colds, “lasting immunity is not conferred” by catching a cold, and children are prone to have multiple colds during a winter season.
In 1961, the American Review of Respiratory Disease published a similar study without that limitation. Shortly before the “Asian influenza epidemic” of 1958, researchers equipped an entire wing of a Veterans Administration Hospital in Livermore, California with UV lights to disinfect the air above people’s heads. This time, the results were even more stunning:
- The epidemic “struck with explosive force during the second and third weeks of January,” producing a “severe, prostrating illness” among 19% of the patients in the non-radiated wings of the hospital.
- Among the hospital staff, 18% also caught the disease.
- The same hospital staff worked in the radiated and non-radiated wings of the hospital, thus potentially carrying the disease into both areas.
- “The radiated patient population was completely spared” with not a single case of the flu among 209 people.
This was not an RCT because the patients were not randomly assigned to the irradiated wing of the hospital, but it approximated one because:
- the vast bulk of patients in all wings had tuberculous or chronic pulmonary disease.
- the irradiated and non-radiated patients had “roughly equal exposure” to the hospital workers, who caught the flu at the same rate as the nonradiated patients.
Like the experiments in schools, the authors of the hospital study emphasized that the indirect UV light would only control the spread of “air-borne” or “aerosolized” particles. This adds to the mountain of evidence that contagious respiratory diseases are mainly spread by aerosols, not droplets or touching common objects.
In 2015, the American Journal of Respiratory and Critical Care Medicine published the results of a controlled trial of upper room UV disinfection on guinea pigs. For this experiment, air was pumped in from a hospital tuberculosis ward to rooms containing 180 guinea pigs. The study found that UV light reduced the odds of infection by 80%.
Some studies have failed to find benefits from upper room UV, but as explained in a 2010 paper in the journal Public Health Reports, the studies were conducted in situations where there was “a high risk of acquiring the same infection outside the location where” the UV was deployed, such as school buses. This is not an issue for places like hospitals and nursing homes, where UV lights can be installed wherever the patients and residents may be.
In addition to upper room systems, UV light can also be used to disinfect air while it passes through heating, ventilation, and air conditioning (HVAC) systems. This is called “in-duct” or “airstream” disinfection.
As well as can be determined without observational studies and RCTs, it appears that in-duct UV reduces the transmission of diseases that are spread by infectious aerosols. This is because lab and field studies have repeatedly found that these systems kill the vast bulk of airborne microbes that flow through them.
Some of the pros and cons of upper room versus in-duct UV systems are as follows:
- When used with fans to increase circulation, upper room UV systems can disinfect the air in a room roughly 57 to 100 times per hour, while the air turnover rates of HVAC systems are typically much lower. In the Washington State Convention Center, for example, the HVAC air turnover rates range from 5.9 to 20.1 times per hour.
- Since in-duct systems are fully enclosed, powerful UV lights can be used without concern for hurting people.
- In buildings that already have HVAC systems, adding in-duct UV is far less expensive to install and operate than upper room UV. On the other hand, upper room systems are more economical than installing a complete HVAC system.
Another option for disinfecting air with UV light is portable in-duct units. These commercial and consumer products are relatively inexpensive, and they can be strategically placed between people in close quarters like roommates and dinner guests. However, studies to measure their effectiveness are lacking. With regard to these matters:
- a 2020 paper in the journal Building and Environment found that “conventional surgical masks are not effective if most infectious viruses are contained in fine droplets [aerosols], and non-conventional intervention methods such as personalized ventilation should be considered as infection prevention strategies given the possible dominance of the short-range airborne route, although further clinical evidence is needed.”
- a 2020 commentary in the journal Clinical Infectious Diseases suggests various measures, including the use of “germicidal ultraviolet lights,” to stem the tide of Covid-19 transmission.
- a 2020 statement by the International Commission on Illumination makes these points:
- “Whilst it is possible to damage some microorganisms and viruses with most of the ultraviolet radiation spectrum, UV-C [with a wavelength of 100–280 nanometers] is the most effective and hence UV-C is most commonly used as GUV [germicidal UV].”
- “Products that emit UV-C are extremely useful in disinfection of air and surfaces or sterilization of water.”
- “Although UVGI [ultraviolet germicidal irradiation] is not considered carcinogenic, its domestic use (for example, consumer products advertised for control of COVID-19) is cautioned against as it requires expert knowledge of the dosage required, and the efficacies of these consumer products are in doubt.”
The CDC is aware of UV disinfection technology but relegates it to a “supplemental treatment” when “options for increasing room ventilation and filtration are limited.” Meanwhile, a note at the top of the same webpage and others on cdc.gov instructs people to “wear a mask indoors in public if you are in an area of substantial or high transmission.” This is yet another example of how the CDC’s myopic agenda on masks is neglecting real opportunities to save lives.
Building Immunity
Another area of tunnel vision for the CDC and other government agencies is their focus on limiting Covid-19 cases, as opposed to deaths. The ramifications of this are quantified in a study published by the British Medical Journal in 2020, which found these stunning and “counterintuitive results”:
- UK policymakers implemented a Covid-19 lockdown based on advice that was focused “on reducing total number of cases and not the number of deaths.”
- Like many other nations, the advice used to justify lockdowns in the UK came from the Imperial College of London, which “contrary to popular perception,” never “specifically modelled” the lockdown.
- When adjusted to reflect high transmissibility of C-19, the Imperial College model projects that once some basic preventative measures are in place like quarantining infected people and social distancing for the elderly:
- the “closure of schools and universities would increase the total number of deaths.”
- “general social distancing” of the entire population “was also projected to increase the total number of deaths.”
- “postponing the spread of Covid-19 means that more people are still infectious and are available to infect older age groups, of whom a much larger fraction then die.”
Those outcomes assume a C-19 infection mortality rate of 1% (higher than reality) and that widespread vaccination does not occur for 800 days (slower than reality), but the basic point remains the same: Lockdowns to control the spread of C-19 can actually cause more C-19 deaths by preventing the development of herd immunity among healthy people—the vast majority of whom are very resilient to the virus.
Those avoidable C-19 deaths are in addition to hordes of other deaths caused in the short run and long term by lockdown-induced depression, anxiety, missed medical care, unemployment, and poverty.
Scholarly Reviews
Just Facts asked several scholars who specialize in the disciplines addressed in this research to critically review it. Among those who did so, they assessed it as follows:
“This research is truly impressive, accurate, and important. Every doctor, nurse, parent, policymaker, and public servant should carefully read and act in accord with it. Overconfidence in the effectiveness of masks is dangerous, and it causes people to not recognize when masks are appropriate and how to properly use them. Further, mask mandates that are at odds with scientific facts are leading to widespread distrust that has long-term ramifications for public health.”
– Dr. Rodney Sturdivant, Ph.D. in Biostatistics, Director of the Statistical Consulting Center at Baylor University
“The sections of this research on social bonds and communication, which are among my primary areas of clinical expertise, are spot on and illuminate what I diagnose on an alarmingly regular basis. I look forward to the publication of this article, so I can share it with all of my patients.”
– Dr. Joseph P. Damore, Jr., M.D., Diplomate, American Board of Psychiatry and Neurology in General Psychiatry and Child and Adolescent Psychiatry
– – –
James D. Agresti is the president of Just Facts, a think tank dedicated to publishing rigorously documented facts about public policy issues.