by Greg Piper
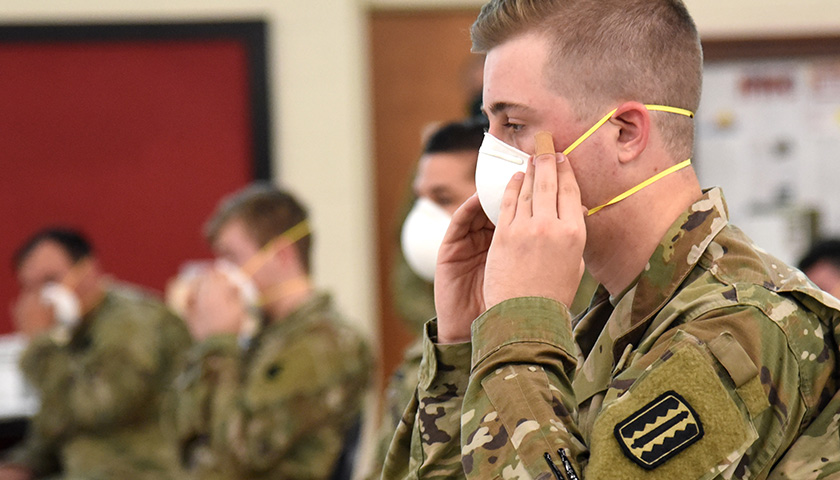
The CDC took nearly two years to formally recognize distinctions between masks for mitigating COVID-19 spread, finally saying in January that cloth masks offer “the least” protection and N95 respirators, which meet strict federal standards, “the highest.”
The agency’s slight nod to the largely symbolic value of cloth masks, predominantly worn in school settings, followed months of calls by onetime White House COVID advisers, among others, to promote masks actually designed to stop aerosolized transmission. It also spurred a run on N95s, sending prices skyward.
But a new peer-reviewed, randomized controlled trial (RCT) of N95s versus surgical masks, considered the midrange of protection, is undermining the late federal pivot to higher-quality masks and calls to reimpose mask mandates in schools, among other settings.
Published in the Annals of Internal Medicine (AIM) this week and led by researchers at Canada’s McMaster University, the study found no statistically significant difference in protection between the two kinds of masks in healthcare facilities in Canada, Israel, Pakistan and Egypt.
Funders included the Canadian government and World Health Organization, which unlike the U.S. opposes masking young children and also found “no evidence” face coverings made a difference against influenza in a 2019 study.
Previous RCTs in the COVID era have found mediocre protection from face coverings at best. A Danish study of 6,000 that had trouble getting published — and eventually landed in AIM — found no statistically significant difference between surgical and no-mask wearers.
A much larger Bangladeshi study led by Yale researchers found that villages that got surgical masks reduced symptomatic infection by 11%, but the confidence interval hit zero and statistical significance disappeared for every age group under 50. Cloth masks had an “imprecise zero” effect.
Missouri Attorney General Eric Schmitt claimed that retiring National Institute of Allergy and Infectious Diseases Director Anthony Fauci, whose flip-flops on masking led to mass public confusion early in the pandemic, couldn’t name any studies showing mask effectiveness in his recent deposition in state-led litigation against alleged federal censorship.
Another tidbit from Fauci depo: In Feb ‘20 he emailed a friend advising her masks were ineffective. Confirmed again on Mar 31. On Apr 3 he’s adamant masks should be worn even though he couldn’t cite a single study to prove it. Mandates followed—Lives ruined
COVID tyranny is born
— Eric Schmitt (@Eric_Schmitt) November 25, 2022
Lawyer Jenin Younes, whose New Civil Liberties Alliance joined Schmitt and Louisiana AG Jeff Landry in the litigation, told The Epoch Times Fauci also couldn’t cite what “studies or study changed his mind in that interim” between his private opposition to masking in February 2020 and public embrace of masking in April.
The McMaster study enrolled about a thousand healthcare workers from May 2020 through March 2022 “who provided direct care to patients with suspected or confirmed COVID-19” and pledged to wear either “fit-tested” N95s or surgical masks for 10 weeks at all times in their facilities. Weekly self-reporting was backed by “external monitoring wherever feasible” and occasional audits.
Workers were excluded if they didn’t have “a valid fit test within the past 24 months or could not pass a fit test,” had at least one high-risk COVID comorbidity, had previous lab-confirmed COVID or had received one or more COVID vaccine doses “with greater than 50% efficacy for the circulating strain” — excluding lower-quality vaccines common abroad.
The infection rate in the N95 group was 9.27%, and the surgical, 10.46%. The former suffered a slightly higher rate of adverse events — discomfort, headache and skin irritation — from wearing the coverings (13.6%) than did the latter (10.8%).
The University of Minnesota’s Center for Infectious Disease Research and Policy, led by former White House COVID adviser Michael Osterholm — a strong booster of N95s — published a report that tried to discredit the findings.
It emphasized the surgical group wore N95s during “aerosol-generating procedures,” infections may have occurred outside the hospital, and only 81% of the N95 group reported wearing them “all the time.”
“We just don’t need another poorly designed and conducted study on this,” Osterholm said in CIDRAP’s report, claiming that N95s’ superiority over surgical masks was already settled.
A multi-national RCT is not just limited but useless and crazy. We should ignore it. A case report from the Chinese government, though? Immediately actionable.
Why does EBM+ just remind me of motivated reasoning? pic.twitter.com/kk59HCm3Vg
— Benjamin Mazer (@BenMazer) November 29, 2022
“It’s really crazy to see the same people who claimed that n95’s were a ‘parachute'” — an intervention so obvious it needs no control group — “to argue this trial was underpowered,” tweeted University of California San Francisco epidemiologist Vinay Prasad, coauthor of an earlier meta-review of mask research that included cloth and surgical. “According to ‘physics’ there should have been no infections in the n95 group, right?
“Truth is actual behavior interventions (like masking) generally fail.”
Watching Twitter peer review this article is like watching cooking with a dull knife. Painful.
It's sad how many doctors base their decisions on their naked political preference, and are unable to actually read the literature. https://t.co/rrdlFEk4qu
— Vinay Prasad MD MPH (@VPrasadMDMPH) December 1, 2022
The study really shows the difference between theory and real-world practice, some observers claimed.
“If N95s are more effective in long Twitter rants (EBM+) than in pragmatic randomized controlled trials (EBM), it might be time to move on and focus on other interventions,” Johns Hopkins epidemiologist Stefan Baral tweeted, referring to evidence-based medicine supplemented by “mechanistic evidence” and true EBM.
“As one doctor told me, ‘If you can wear an N95 for more than about 30 minutes you are wearing it wrong,'” tweeted George Mason University law professor Todd Zywicki, who successfully challenged GMU’s COVID vaccine mandate in court.
“Also illustrates that mechanistic evidence (here, of N95 superior filtration) doesn’t always = real-world significance,” lawyer and COVID policy critic Newman Nahas tweeted.
The weak findings from the most rigorous studies haven’t extinguished enthusiasm for mask mandates, particularly in schools, despite warnings from the FDA and 3M not to jury-rig N95s on kids.
A recent op-ed in MedPage Today claimed school masking could “reduce the burden on our healthcare system” in the face of the theorized but vigorously disputed “tripledemic” of COVID, flu and RSV. The authors cited a heavily confounded observational study of Massachusetts schools after its state mask mandate ended.
The Department of Health and Human Services commissioned a study by consulting firm Coforma that claimed the reimposition of mask mandates and social distancing could ease the risks to purported sufferers of long COVID, studies of which have found no obvious biochemical markers and disproportionate reporting by white, educated women.
The Coforma study didn’t cite any research for mask effectiveness or distinguish by mask type, however, and the HHS press release left out its call to “encourage or mandate” mask-wearing. The agency emphasized to the New York Post it wasn’t recommending mask mandates.
High mask-wearing rates have seemingly not made a difference in Japan, where infection rates are substantially higher than those in the less-masked U.S. despite far less COVID testing in the former.
Seems to be working well pic.twitter.com/7xfqn2VMTg
— Mitch Lowe 🇵🇱 (@Mitch___Lowe) December 1, 2022
– – –
Greg Piper has covered law and policy for 15 years, with a focus on tech companies, civil liberties and higher education.
Photo “Virginia National Guard Soldiers Learn How to Perform N95 Respirator Mask Fit Tests” by Virginia Guard Public Affairs. CC BY-NC 2.0.

Sign up here to get your copy of The Star News Network Daily Update
Daily updates, breaking news, special offers, and more